 |
|
|||||||
| Sexual Health Issues If you need medical advice regarding your sexual health, ask Dr Tan. We are honored to have an In House Doctor who is here to help. |
 |
|
|
Thread Tools |
|
#1
|
||||
|
||||
|
All you need to know about Herpes
Herpes Support Group for Ladies - click this link
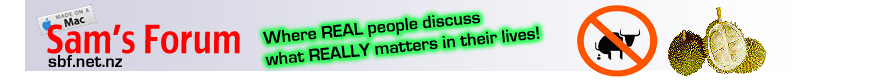
Herpes simplex - wikipedia part 1 Source: http://en.wikipedia.org/wiki/Herpes_simplex Herpes simplex (Ancient Greek: ἕρπης - herpes, lit. "creeping") is a viral disease caused by both herpes simplex virus type 1 (HSV-1) and type 2 (HSV-2). Infection with the herpes virus is categorized into one of several distinct disorders based on the site of infection. Oral herpes, the visible symptoms of which are colloquially called cold sores or fever blisters, infects the face and mouth. Oral herpes is the most common form of infection. Genital herpes, known simply as herpes, is the second most common form of herpes. Other disorders such as herpetic whitlow, herpes gladiatorum, ocular herpes (keratitis), cerebral herpes infection encephalitis, Mollaret's meningitis, neonatal herpes, and possibly Bell's palsy are all caused by herpes simplex viruses. Herpes viruses cycle between periods of active disease—presenting as blisters containing infectious virus particles—that last 2–21 days, followed by a remission period. Genital herpes, however, is often asymptomatic, though viral shedding may still occur. After initial infection, the viruses are transported along sensory nerves to the sensory nerve cell bodies, where they become latent and reside life-long. Causes of recurrence are uncertain, though some potential triggers have been identified, including immunosuppressant drugs (see below). The previously latent virus then multiplies new virus particles in the nerve cell and these are transported along the axon of each neuron to the nerve terminals in the skin, where they are released. Over time, episodes of active disease reduce in frequency and severity. Herpes simplex is most easily transmitted by direct contact with a lesion or the body fluid of an infected individual. Transmission may also occur through skin-to-skin contact during periods of asymptomatic shedding. Barrier protection methods are the most reliable method of preventing transmission of herpes, but they merely reduce rather than eliminate risk. Oral herpes is easily diagnosed if the patient presents with visible sores or ulcers. Early stages of orofacial herpes and genital herpes are harder to diagnose; laboratory testing is usually required. A cure for herpes has not yet been developed. Once infected, the virus remains in the body for life. However, after several years, some people will become perpetually asymptomatic and will no longer experience outbreaks, though they may still be contagious to others. Treatments with antivirals can reduce viral shedding and alleviate the severity of symptomatic episodes. Vaccines are in clinical trials but have not demonstrated effectiveness. It should not be confused with conditions caused by other viruses in the herpesviridae family such as herpes zoster, which is caused by varicella zoster virus. The differential diagnosis includes hand, foot and mouth disease due to similar lesions on the skin. Classification Herpes simplex is divided into two types: HSV type 1 and HSV type 2. HSV1 primarily causes mouth, throat, face, eye, and central nervous system infections, while HSV2 primarily causes anogenital infections.[1] However, each may cause infections in all areas. Signs and symptoms HSV infection causes several distinct medical disorders. Common infection of the skin or mucosa may affect the face and mouth (orofacial herpes), genitalia (genital herpes), or hands (herpes whitlow). More serious disorders occur when the virus infects and damages the eye (herpes keratitis), or invades the central nervous system, damaging the brain (herpes encephalitis). Patients with immature or suppressed immune systems, such as newborns, transplant recipients, or AIDS patients are prone to severe complications from HSV infections. HSV infection has also been associated with cognitive deficits of bipolar disorder,[2] and Alzheimer's disease,[3] although this is often dependent on the genetics of the infected person. In all cases HSV is never removed from the body by the immune system. Following a primary infection, the virus enters the nerves at the site of primary infection, migrates to the cell body of the neuron, and becomes latent in the ganglion. As a result of primary infection, the body produces antibodies to the particular type of HSV involved, preventing a subsequent infection of that type at a different site. In HSV-1 infected individuals, seroconversion after an oral infection will prevent additional HSV-1 infections such as whitlow, genital herpes, and keratitis. Prior HSV-1 seroconversion seems to reduce the symptoms of a later HSV-2 infection, although HSV-2 can still be contracted. Most indications are that an HSV-2 infection contracted prior to HSV-1 seroconversion will also immunize that person against HSV-1 infection.[citation needed] Many people infected with HSV-2 display no physical symptoms—individuals with no symptoms are described as asymptomatic or as having subclinical herpes.  Bell's palsy Although the exact cause of Bell's palsy, a type of facial paralysis, is unknown it may be related to reactivation of herpes simplex virus type 1. This theory has been contested, however since HSV is detected in large numbers of individuals who never experienced facial paralysis, and higher levels of antibodies for HSV are not found in HSV-infected individuals with Bell's palsy compared to those without. Regardless antivirals have been found to not improve outcomes. Alzheimer's disease SV-1 has been proposed as a possible cause of Alzheimer's disease.[ In the presence of a certain gene variation (APOE-epsilon4 allele carriers), HSV-1 appears to be particularly damaging to the nervous system and increases one’s risk of developing Alzheimer’s disease. The virus interacts with the components and receptors of lipoproteins, which may lead to the development of Alzheimer's disease. Without the presence of the gene allele, HSV type 1 does not appear to cause any neurological damage and thus increase the risk of Alzheimer’s. Herpes simplex virus type 1 DNA is localized within the beta-amyloid plaques that characterize Alzheimer's disease. It suggests that this virus is a major cause of the plaques and hence probably a significant aetiological factor in Alzheimer's disease. Pathophysiology Herpes is contracted through direct contact with an active lesion or body fluid of an infected person. Herpes transmission occurs between discordant partners; a person with a history of infection (HSV seropositive) can pass the virus to an HSV seronegative person. The only way to contract Herpes simplex virus 2 is through direct skin-to-skin contact with an infected individual.[citation needed] To infect a new individual, HSV travels through tiny breaks in the skin or mucous membranes in the mouth or genital areas. Even microscopic abrasions on mucous membranes are sufficient to allow viral entry. HSV asymptomatic shedding occurs at some time in most individuals infected with herpes. It can occur more than a week before or after a symptomatic recurrence in 50% of cases. Virus enters into susceptible cells via entry receptors such as nectin-1, HVEM and 3-O sulfated heparan sulfate. Infected people that show no visible symptoms may still shed and transmit virus through their skin; asymptomatic shedding may represent the most common form of HSV-2 transmission. Asymptomatic shedding is more frequent within the first 12 months of acquiring HSV. Concurrent infection with HIV increases the frequency and duration of asymptomatic shedding. There are indications that some individuals may have much lower patterns of shedding, but evidence supporting this is not fully verified; no significant differences are seen in the frequency of asymptomatic shedding when comparing persons with one to twelve annual recurrences to those who have no recurrences. Antibodies that develop following an initial infection with a type of HSV prevents reinfection with the same virus type—a person with a history of orofacial infection caused by HSV-1 cannot contract herpes whitlow or a genital infection caused by HSV-1. In a monogamous couple, a seronegative female runs a greater than 30% per year risk of contracting an HSV infection from a seropositive male partner.[24] If an oral HSV-1 infection is contracted first, seroconversion will have occurred after 6 weeks to provide protective antibodies against a future genital HSV-1 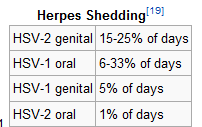 
__________________
You are my forum, my only forum, you make me happy, when skies are grey... Sex health related questions click here. WOMEN'S CHARTER click here Sg law on sex related matters click here Last edited by Big Sexy; 27-01-2016 at 09:04 AM. |
|
#2
|
||||
|
||||
|
Re: All you need to know about Gential Herpes
Herpes simplex - wikipedia part 2
Source: http://en.wikipedia.org/wiki/Herpes_simplex Diagnosis Primary orofacial herpes is readily identified by clinical examination of persons with no previous history of lesions and contact with an individual with known HSV-1 infection. The appearance and distribution of sores in these individuals typically presents as multiple, round, superficial oral ulcers, accompanied by acute gingivitis. Adults with non-typical presentation are more difficult to diagnose. Prodromal symptoms that occur before the appearance of herpetic lesions help differentiate HSV symptoms from the similar symptoms of other disorders, such as allergic stomatitis. When lesions do not appear inside the mouth, primary orofacial herpes is sometimes mistaken for impetigo, a bacterial infection. Common mouth ulcers (aphthous ulcer) also resemble intraoral herpes, but do not present a vesicular stage. Genital herpes can be more difficult to diagnose than oral herpes since most HSV-2-infected persons have no classical symptoms. Further confusing diagnosis, several other conditions resemble genital herpes, including fungal infection, lichen planus, atopic dermatitis, and urethritis. Laboratory testing is often used to confirm a diagnosis of genital herpes. Laboratory tests include: culture of the virus, direct fluorescent antibody (DFA) studies to detect virus, skin biopsy, and polymerase chain reaction (PCR) to test for presence of viral DNA. Although these procedures produce highly sensitive and specific diagnoses, their high costs and time constraints discourage their regular use in clinical practice. Until recently, serological tests for antibodies to HSV were rarely useful to diagnosis and not routinely used in clinical practice. The older IgM serologic assay could not differentiate between antibodies generated in response to HSV-1 or HSV-2 infection. However, the new Immunodot glycoprotein G-specific (IgG) HSV test is more than 98% specific at discriminating HSV-1 from HSV-2. It is the opinion of some modern medical professionals that the new IgG test should always be clinically preferred to the old IgM test, however not all doctors appear to be informed of the availability of the newer, reliable IgG tests. Barrier methods Condoms offer moderate protection against HSV-2 in both men and women, with consistent condom users having a 30% lower risk of HSV-2 acquisition compared with those who never use condoms The virus cannot pass through a latex condom, but a condom's effectiveness is limited because[citation needed] it does not prevent skin contact or bodily fluid contact with the scrotum, anus, buttocks, upper thighs or area immediately surrounding the penis, all of which are susceptible to infection with and transmission of the virus. Preventing contact with these areas during sex, in addition to wearing a condom, should theoretically provide enhanced protection against herpes.[original research?] The use of condoms or dental dams also limits the transmission of herpes from the genitals of one partner to the mouth of the other (or vice versa) during oral sex. When one partner has a herpes simplex infection and the other does not, the use of antiviral medication, such as valaciclovir, in conjunction with a condom, further decreases the chances of transmission to the uninfected partner. Topical microbicides which contain chemicals that directly inactivate the virus and block viral entry are being investigated. Vaccine Vaccines for HSV are undergoing trials. Once developed, they may be used to help with prevention or minimize initial infections as well as treatment for existing infections Antivirals Antivirals may reduce asymptomatic shedding; it is believed asymptomatic genital HSV-2 viral shedding occurs on 20% of days per year in patients not undergoing antiviral treatment, versus 10% of days while on antiviral therapy Pregnancy The risk of transmission from mother to baby is highest if the mother becomes infected at around the time of delivery (30% to 60%), but the risk falls to 3% if it is a recurrent infection, and is less than 1% if there are no visible lesions. To prevent neonatal infections, seronegative women are recommended to avoid unprotected oral-genital contact with an HSV-1 seropositive partner and conventional sex with a partner having a genital infection during the last trimester of pregnancy. A seronegative mother who contracts HSV at this time has up to a 57% chance of conveying the infection to her baby during childbirth, since insufficient time will have occurred for the generation and transfer of protective maternal antibodies before the birth of the child, whereas a woman seropositive for both HSV-1 and HSV-2 has around a 1-3% chance of transmitting infection to her infant. Women who are seropositive for only one type of HSV are only half as likely to transmit HSV as infected seronegative mothers. Mothers infected with HSV are advised to avoid procedures that would cause trauma to the infant during birth (e.g. fetal scalp electrodes, forceps, and vacuum extractors) and, should lesions be present, to elect caesarean section to reduce exposure of the child to infected secretions in the birth canal. The use of antiviral treatments, such as acyclovir, given from the 36th week of pregnancy, limits HSV recurrence and shedding during childbirth, thereby reducing the need for caesarean section. Acyclovir is the recommended antiviral for herpes suppressive therapy during the last months of pregnancy. The use of valaciclovir and famciclovir, while potentially improving compliance have less well determined safety in pregnancy. Treatment There is no method to eradicate herpes virus from the body, but antiviral medications can reduce the frequency, duration, and severity of outbreaks. Analgesics such as ibuprofen and acetaminophen can reduce pain and fever. Topical anesthetic treatments such as prilocaine, lidocaine, benzocaine or tetracaine can also relieve itching and pain Antiviral There are several antivirals that are effective for treating herpes including: aciclovir (acyclovir), valaciclovir (valacyclovir), famciclovir, and penciclovir. Aciclovir was the first discovered and is now available in generic. Evidence supports the use of aciclovir and valaciclovir in the treatment of herpes labialis. as well as herpes infections in people with cancer. The evidence to support the use of acyclovir in primary herpetic gingivostomatitis is less strong. Topical A number of topical antivirals are effective for herpes labialis including acyclovir, penciclovir, and docosanol. Docosanol can be purchased over the counter in Canada and the USA. Alternative medicine Certain dietary supplements and alternative remedies are claimed to be beneficial in the treatment of herpes. There is however insufficient evidence to support use of many of these compounds including echinacea, eleuthero, L-lysine, zinc, bee products and aloe vera. A single study indicates possible benefit from laser treatment.  
__________________
You are my forum, my only forum, you make me happy, when skies are grey... Sex health related questions click here. WOMEN'S CHARTER click here Sg law on sex related matters click here Last edited by Big Sexy; 27-01-2016 at 09:06 AM. |
|
#3
|
||||
|
||||
|
Re: All you need to know about Gential Herpes
Herpes simplex - wikipedia part 3
Source: http://en.wikipedia.org/wiki/Herpes_simplex Prognosis Following active infection, herpes viruses establish a latent infection in sensory and autonomic ganglia of the nervous system. The double-stranded DNA of the virus is incorporated into the cell physiology by infection of the nucleus of a nerve's cell body. HSV latency is static—no virus is produced—and is controlled by a number of viral genes, including Latency Associated Transcript (LAT). Many HSV-infected people experience recurrence within the first year of infection. Prodrome precedes development of lesions. Prodromal symptoms include tingling (paresthesia), itching, and pain where lumbosacral nerves innervate the skin. Prodrome may occur as long as several days or as short as a few hours before lesions develop. Beginning antiviral treatment when prodrome is experienced can reduce the appearance and duration of lesions in some individuals. During recurrence, fewer lesions are likely to develop, lesions are less painful and heal faster (within 5–10 days without antiviral treatment) than those occurring during the primary infection. Subsequent outbreaks tend to be periodic or episodic, occurring on average four to five times a year when not using antiviral therapy. The causes of reactivation are uncertain, but several potential triggers have been documented. A recent study (2009) showed that the protein VP16 plays a key role in reactivation of the dormant virus. Changes in the immune system during menstruation may play a role in HSV-1 reactivation. Concurrent infections, such as viral upper respiratory tract infection or other febrile diseases, can cause outbreaks. Reactivation due to infection is the likely source of the historic terms cold sore and fever blister. Other identified triggers include: local injury to the face, lips, eyes, or mouth, trauma, surgery, radiotherapy, and exposure to wind, ultraviolet light, or sunlight. The frequency and severity of recurrent outbreaks vary greatly between patients. Some individuals' outbreaks can be quite debilitating with large, painful lesions persisting for several weeks, while others will experience only minor itching or burning for a few days. There is some evidence that genetics plays a role in the frequency of cold sore outbreaks. An area of human chromosome 21 that includes 6 genes has been linked to frequent oral herpes outbreaks. An immunity to the virus is built over time. Most infected individuals will experience fewer outbreaks and outbreak symptoms will often become less severe. After several years, some people will become perpetually asymptomatic and will no longer experience outbreaks, though they may still be contagious to others. Immuno-compromised individuals may experience episodes that are longer, more frequent, and more severe. Antiviral medication has been proven to shorten the frequency and duration of outbreaks. Outbreaks may occur at the original site of the infection or in proximity to nerve endings that reach out from the infected ganglia. In the case of a genital infection, sores can appear at the original site of infection or near the base of the spine, the buttocks, or the back of the thighs. HSV-2 infected individuals are at higher risk for acquiring HIV when practicing unprotected sex with HIV-positive persons, particularly during an outbreak with active lesions. Epidemiology Worldwide rates of HSV infection are between 65% and 90%. HSV1 is more common than HSV2 with rates of both increasing as people age. Rates of infection are determined by the presence of antibodies against either viral species. In the US, 57.7% of the population is infected with HSV-1 and 16.2% are infected with HSV-2. Among those HSV-2 seropositive, only 18.9% were aware that they were infected History Herpes has been known for at least 2,000 years. It is said that Emperor Tiberius banned kissing in Rome for a time due to so many people having cold sores. In the 16th century Romeo and Juliet, it is mentioned that there are blisters "o'er ladies' lips." In 18th century it was so common among prostitutes that it was called "a vocational disease of women."[66] The term Herpes Simplex appeared in Richard Boulton's A System of Rational and Practical Chirurgery in 1713, where the terms Herpes miliaris and Herpes exedens also appeared. Herpes was not found to be a virus until the 1940s.[66] Herpes antiviral therapy began in the early 1960s with the experimental use of medication that interfered with viral replication called deoxyribonucleic acid (DNA) inhibitors. The original use was against normally fatal or disabilitating illness such as adult encephalitis, keratitis, in immunocompromised (transplant) patients, or disseminated herpes zoster.[70] The original compounds used were 5-iodo-2'-deoxyuridine, AKA idoxuridine, IUdR, or(IDU) and 1-β-D-arabinofuranosylcytosine or ara-C, later marketed under the name cytosar or cytorabine. The usage expanded to include topical treatment of herpes simplex, zoster, and varicella. Some trials combined different antivirals with differing results. The introduction of 9-β-D-arabinofuranosyladenine, AKA ara-A or vidarabine, considerably less toxic than Ara-C, in the mid 1970s, heralded the way for the beginning of regular neonatal antiviral treatment. Vidarabine was the first systemically administered antiviral medication with activity against HSV for which therapeutic efficacy outweighed toxicity for the management of life-threatening HSV disease. Intravenous vidarabine was licensed for use by the U.S. Food and Drug Administration (FDA) in 1977. Other experimental antivirals of that period included: Heparin, trifluorothymidine (TFT),[ Ribivarin, interferon, Virazole, and 5-methoxymethyl-2'-deoxyuridine (MMUdR).] The introduction of 9-(2-hydroxyethoxymethyl)guanine, AKA acyclovir, in the late 1970s raised antiviral treatment another notch and led to vidarabine vs. acyclovir trials in the late 1980s. The lower toxicity and ease of administration over vidarabine has led to acyclovir becoming the drug of choice for herpes treatment after it was licensed by the FDA in 1998. Another advantage in the treatment of neonatal herpes included greater reductions in mortality and morbidity with increased dosages, something that did not occur when compared with increased dosages of vidarabine.[82] On the other side of the equation, acyclovir seems to inhibit antibody response and newborns on acyclovir antiviral treatment experienced a slower rise in antibody titer than those on vidarabine.   
__________________
You are my forum, my only forum, you make me happy, when skies are grey... Sex health related questions click here. WOMEN'S CHARTER click here Sg law on sex related matters click here Last edited by Big Sexy; 07-05-2011 at 09:24 PM. |
|
#4
|
||||
|
||||
|
Re: All you need to know about Gential Herpes
Herpes simplex - wikipedia part 4
Source: http://en.wikipedia.org/wiki/Herpes_simplex Society and culture Herpes simplex was not always stigmatised. It was merely a cold sore in an unusual place until the 1970s. As late as 1975, a study of “Psychological morbidity in a clinic for sexually-transmitted disease” (Richard Mayou, The London Hospital) [83] does not mention herpes simplex because at that time, there was no significant morbidity problem (i.e. mental anxiety or illness) associated with the virus. In the Journal of Clinical Investigation,[84] Pedro Cuatrecasas states, “during the R&D of acyclovir (Zovirax), marketing [department of Burroughs Wellcome] insisted that there were ‘no markets’ for this compound. Most had hardly heard of genital herpes...” Thus marketing the medical condition – separating the ‘normal cold sore’ from the ‘stigmatized genital infection’ was to become the key to marketing the drug, a process now known as ‘disease mongering’ [85] Since the creation of the herpes hype, some people experience negative feelings related to the condition following diagnosis, particularly if they have acquired the genital form of the disease. Feelings can include depression, fear of rejection, feelings of isolation, fear of being found out, self-destructive feelings, and fear of masturbation.[86] These feelings usually lessen over time. Much of the hysteria and stigma surrounding herpes stems from a media campaign beginning in the late 1970s and peaking in the early 1980s. There were multiple articles worded in fear-mongering and anxiety-provoking terminology, such as the now ubiquitous "attacks," "outbreaks," "victims," and "sufferers." At one point the term "herpetic" even entered the popular lexicon. The articles were published by Reader's Digest, U.S. News, and Time magazine, among others. A made-for-TV movie was named Intimate Agony. The peak was when Time magazine had 'Herpes: The New Scarlet Letter' on the cover in August 1982, forever stigmatizing the word in the public mind.[66] The scientific reality is that most people are asymptomatic, the virus causes no real health problems for a vast majority of people, and a vast majority (around 90%) of the Earth's population carries HSV-1, 2, or both.[87][88] Herpes support groups have been formed in the United States and the UK, providing information about herpes and running message forums and dating websites for "sufferers." People with the herpes virus are often hesitant to divulge to other people, including friends and family, that they are infected. This is especially true of new or potential sexual partners whom they consider casual Research Researchers at the University of Florida have made a hammerhead ribozyme that targets and cleaves the mRNA of essential genes in HSV-1. The hammerhead which targets the mRNA of the UL20 gene greatly reduced the level of HSV-1 ocular infection in rabbits and reduced the viral yield in vivo.[90] The gene-targeting approach uses a specially designed RNA enzyme to inhibit strains of the herpes simplex virus. The enzyme disables a gene responsible for producing a protein involved in the maturation and release of viral particles in an infected cell. The technique appears to be effective in experiments with mice and rabbits, but further research is required before it can be attempted in people who are infected with herpes.[91] Another possibility to eradicate the HSV-1 variant is being pursued by a team at Duke University. By figuring out how to switch all copies of the virus in the host from latency to their active stage at the same time, rather than the way the virus copies normally stagger their activity stage, leaving some dormant somewhere at all times, it is thought that conventional anti-viral drugs can kill the entire virus population completely, since they can no longer hide in the nerve cells. One class of drugs called antagomir could serve this purpose. These are chemically engineered oligonucleotides or short segments of RNA, that can be made to mirror their target genetic material, namely herpes microRNAs. They could be engineered to attach and thus 'silence' the microRNA, thus rendering the virus incapable to keep latent in their host.[92] Professor Cullen believes a drug could be developed to block the microRNA whose job it is to suppress HSV-1 into latency.[93] One vaccine that was under trial was Herpevac, a vaccine against HSV-2. The National Institutes of Health (NIH) in the United States conducted phase III trials of Herpevac.[94] In 2010, it was reported that, after 8 years of study in more than 8000 women in the United States and Canada, there was no sign of positive results against the sexually transmitted disease caused by HSV-2[95] (and this despite earlier favorable interim reports[94]). A laboratory at Harvard Medical School has developed dl5-29 (now known as ACAM-529), a replication-defective mutant virus that has proved successful both in preventing HSV-2/HSV-1 infections, and in combating the virus in already infected hosts, in animal models. It has been shown that the replication-defective vaccine induces strong HSV-2-specific antibody and T-cell responses; protects against challenge with a wild-type HSV-2 virus; greatly reduces the severity of recurrent disease; provides cross-protection against HSV-1, and renders the virus unable to revert to a virulent state or to become latent.[96] His vaccine is now being researched and developed by Accambis (acquired by Sanofi Pasteur in September 2008), and is due to be applied as an Investigational New Drug in 2009.[97] However, the status of ACAM-529 became after the acquisition somewhat unclear. According to Jim Tartaglia, a company representative of Sanofi Pasteur, ACAM-529 is still under development and should be enter phase I clinical testing in 2012. [98] A private company called BioVex began Phase I clinical trials for ImmunoVEX, another proposed vaccine, in March 2010.[99] A completely new approach has the "HSV-2 ICP0 live-attenuated HSV-2 vaccine" investigated by Dr. William Halford at the Southern Illinois University (SIU) School of Medicine. 
__________________
You are my forum, my only forum, you make me happy, when skies are grey... Sex health related questions click here. WOMEN'S CHARTER click here Sg law on sex related matters click here Last edited by Big Sexy; 27-01-2016 at 09:25 AM. |
|
#5
|
||||
|
||||
|
Re: All you need to know about Gential Herpes
Herpes
Source: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001860/ Source: http://www.cdc.gov/std/herpes/stdfact-herpes.htm Genital herpes is a sexually transmitted viral infection affecting the skin or mucous membranes of the genitals. Causes, incidence, and risk factors Genital herpes is caused by two viruses: *Herpes simplex virus type 2 (HSV-2) *Herpes simplex virus type 1 (HSV-1) Herpes simplex virus type 2 (HSV-2) causes most cases of genital herpes. HSV-2 can be spread through secretions from the mouth or genitals. Herpes simplex virus type 1 (HSV-1) most often causes herpes infections of the mouth and lips (commonly called cold sores or fever blisters). HSV-1 can spread from the mouth to the genitals during oral sex. Herpes simplex virus (HSV) is spread from one person to another during sexual contact. You may be infected with herpes when your skin, vagina, penis, or mouth comes into contact with someone who already has herpes. Herpes is most likely to be transmitted by contact with the skin of an infected person who has visible sores, blisters, or a rash (an active outbreak), but you can also catch herpes from an infected person's skin when they have NO visible sores present (and the person may not even know that he or she is infected), or from an infected persons mouth (saliva) or vaginal fluids. Because the virus can be spread even when there are no symptoms or sores present, a sexual partner who has been infected with herpes in the past but has no active herpes sores can still pass the infection on to others. Genital HSV-2 infections is more common in women (approximately 1 of every 4 women is infected) than it is in men (nearly 1 of every 8 men is infected). Symptoms Many people with HSV-2 infection never have sores, or they have very mild symptoms that they do not even notice or mistake for insect bites or another skin condition. If signs and symptoms do occur during the first outbreak, they can be quite severe. This first outbreak usually happens within 2 weeks of being infected. Generalized or whole-body (systemic) symptoms may include: * Decreased appetite * Fever * General sick feeling (Malaise) * Muscle aches in the lower back, buttocks, thighs, or knees Genital symptoms include the appearance of small, painful blisters filled with clear or straw-colored fluid. They are usually found: * In women: on the outer vaginal lips (labia), vagina, cervix, around the anus, and on the thighs or buttocks * In men: on the penis, scrotum, around the anus, on the thighs or buttocks * In both sexes: on the tongue, mouth, eyes, gums, lips, fingers, and other parts of the body * Before the blisters appear, the person may feel the skin tingling, burning, itching, or have pain at the site where the blisters will appear * When the blisters break, they leave shallow ulcers that are very painful. These ulcers eventually crust over and slowly heal over 7 - 14 days or more Other symptoms that may occur include: * Enlarged and tender lymph nodes in the groin during an outbreak * Painful urination * Women may have vaginal discharge or, occasionally, be unable to empty the bladder and require a urinary catheter A second outbreak can appear weeks or months after the first. It is almost always less severe and shorter than the first outbreak. Over time, the number of outbreaks tends to decrease. Once a person is infected, however, the virus hides within nerve cells and remains in the body. The virus can remain "asleep" (dormant) for a long period of time (this is called latency). The infection can flare-up or reactivate at any time. Events that can trigger latent infection to become active and bring on an outbreak include: * Fatigue * Genital irritation * Menstruation * Physical or emotional stress * Trauma Attacks can recur as seldom as once per year, or so often that the symptoms seem continuous. Recurrent infections in men are generally milder and shorter than those in women. Signs and tests Tests can be done on skin sores or blisters to diagnose herpes. These tests are most often done when someone has a first outbreak and when a pregnant women develops genital herpes symptoms. * Culture of fluid from a blister or open sore may be positive for herpes simplex virus. The herpes simplex virus can in the culture in 2-3 days. It is most useful during the first outbreak. * A test called PCR performed on fluid from a blister shows small amounts of DNA. It is the most accurate test to tell whether the herpes virus is present in the blister. * Blood tests check for antibody levels to the herpes virus. These blood tests can identify whether someone has ever been infected with the herpes virus, even between outbreaks. It may be positive even if they've never had an outbreak. Treatment Genital herpes cannot be cured. However, antiviral medication can relieve pain and discomfort during an outbreak by healing the sores more quickly. These drugs appear to help during first attacks more than they do in later outbreaks. Medicines used to treat herpes include acyclovir, famciclovir, and valacyclovir. For repeat outbreaks, start the medication as soon as the tingling, burning, or itching begins, or as soon as you notice blisters. People who have many outbreaks may take these medications daily over a period of time. This can help prevent outbreaks or shorten their length. It can also reduce the chance of giving herpes to someone else. Pregnant women may be treated for herpes during the last month of pregnancy to reduce the chance of having an outbreak at the time of delivery. If there is an outbreak around the time of delivery, a C-section will be recommended to reduce the chance of infecting the baby. Possible side effects from herpes medications include: * Fatigue * Headache * Nausea and vomiting * Rash * Seizures * Tremor Home care for herpes sores: * Do NOT wear nylon or other synthetic pantyhose, underwear, or pants. Instead, wear loose-fitting cotton garments * Gentle cleansing with soap and water is recommended. * Taking warm baths may relieve the pain (afterward, keep the blisters dry) If one of the sores develops an infection from bacteria, ask your doctor if you need an antibiotic. Expectations (prognosis) Once you are infected, the virus stays in your body for the rest of your life. Some people never have another episode, and others have frequent outbreaks. In most outbreaks, there is no obvious trigger. Many people, however, find that attacks of genital herpes occur with the following conditions: * Fatigue * General illness (from mild illnesses to serious conditions, such as operations, heart attacks, and pneumonia) * Immunosuppression due to AIDS or medication such as chemotherapy or steroids * Menstruation * Physical or emotional stress * Trauma to the affected area, including sexual activity In people with a normal immune system, genital herpes remains a localized and bothersome infection, but is rarely life-threatening.   
__________________
You are my forum, my only forum, you make me happy, when skies are grey... Sex health related questions click here. WOMEN'S CHARTER click here Sg law on sex related matters click here Last edited by Big Sexy; 27-01-2016 at 09:16 AM. |
|
#6
|
||||
|
||||
|
Re: All you need to know about Gential Herpes
Herpes
Source: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001860/ Source: http://www.cdc.gov/std/herpes/stdfact-herpes.htm How common is genital herpes? Results of a nationally representative study show that genital herpes infection is common in the United States. Nationwide, 16.2%, or about one out of six, people 14 to 49 years of age have genital HSV-2 infection. Over the past decade, the percentage of Americans with genital herpes infection in the U.S. has remained stable. Genital HSV-2 infection is more common in women (approximately one out of five women 14 to 49 years of age) than in men (about one out of nine men 14 to 49 years of age). Transmission from an infected male to his female partner is more likely than from an infected female to her male partner. Complications Pregnant women who have an active herpes infection on their genitals or in their birth canal when they deliver may pass the infection to their newborn infant. * The risk of passing the infection to the baby is highest if the mom first becomes infected with herpes during pregnancy. Babies of women who become infected during pregnancy are at risk for premature birth. The baby may develop develop brain infection (meningitis, encephalitis) , chronic skin infeciton, severe developmental delays, or death. * The risk for severe infection in the baby is lower in recurrent outbreaks, with the highest risk in women experiencing an outbreak at the time of delivery. * Women with a history of herpes but who only have occasional or no outbreaks rarely transmit the infection to their babies. Some people may develop severe herpes infections that involve the brain, eyes, esophagus, livere, spinal cord, or lungs. These complications often develop in people who have a weakened immune system, AIDS, are undergoing chemotherapy or radiation therapy, or who take high doses of cortisone. Someone with an active herpes infection who has sexual contact with someone who is HIV positive is more likely to contract HIV infection themselves. Calling your health care provider Call for an appointment with your health care provider if you have any symptoms of genital herpes, or if you develop fever, headache, vomiting, or widespread symptoms during or after an outbreak of herpes. Also call if you are unable to urinate. Prevention The best way to avoid getting genital herpes is to avoid all sexual contact, including oral sex. Next best is being in a long-term, mutually monogamous relationshipw with someone who has been tested and is not, and never has been, infected with herpes. Condoms remain the best way to protect against catching genital herpes during sexual activity with someone who is infected. Using a condom correctly and consistently will help prevent the spread of the disease. * Only latex condomes will work to prevent infection. Animal membrane (sheepskin) condoms won't work because the virus can go right through them. * The female condom has been tested and shown to reduce the risk of trasmitting herpes, as well. * A latex condom should be used during ALL sexual contact, even if the infected person does not have any sores or blisters at that time. In addition, people with genital herpes who don't have any current symptoms should tell their partner that they have the disease. Vaccines against herpes have been developed but are still experimental. 
__________________
You are my forum, my only forum, you make me happy, when skies are grey... Sex health related questions click here. WOMEN'S CHARTER click here Sg law on sex related matters click here Last edited by Big Sexy; 27-01-2016 at 09:24 AM. |
|
#7
|
||||
|
||||
|
Re: All you need to know about Gential Herpes
Most get herpes as kids
Thursday, 28 l 10 l 2010 Source: Mind Your Body; The Straits Times By: April Chong http://www.healthxchange.com.sg/news...s-as-kids.aspx 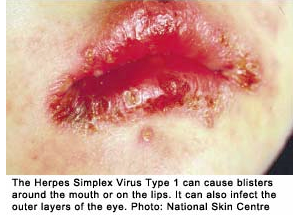 In fact, most people do not know they have it as the infection may have come and gone without any visible symptoms. APRIL CHONG reports People who have never had them do not realise this: cold sores – blisters around the mouth or on the lips – are a common fact of life. They are caused by Herpes Simplex Virus Type 1 and are so prevalent that up to 80 per cent of people would have antibodies against it by the time they reach adulthood. Type 2 is associated with genital herpes. Eight in 10 Type 1 infections would have been probably acquired during childhood, said Dr Tan Hiok Hee, a senior consultant dermatologist at the National Skin Centre. Many people do not know because, in many cases, the infection may have come and gone without any visible symptoms. Aside from the mouth lesions, Herpes Simplex Type 1 can also cause infections of the outer layers of the eye, especially the conjunctiva and cornea. It is transmitted by skin-to-skin contact, such as through infected saliva and direct contact with the sores. Children can get the virus simply by sharing cups, tumbling around during play or getting kissed by an affectionate, but infected, aunt. Once infected, the virus can lie latent in the nerve roots of the infected area and be re-activated to give rise to blisters periodically throughout a person’s life. Triggers include stress and a lowered immune system, said Dr Ng Chung Wai, a consultant family physician at Outram Polyclinic. The virus can also be passed to the genital areas through contact, he added. In fact, cross-infections could occur from oral-genital contact, so that one can get Type 2 infections of the mouth and Type 1 of the genitals. However, oral herpes infections are rarely serious or fatal except when the virus attacks certain areas, such as the brain in extremely ill or vulnerable people, said Dr Tan. While the virus can never be completely eradicated, anti-viral creams and oral anti-viral medications can shorten the duration of the attacks. To prevent your child from catching the virus, teach him not to share items that come into contact with the mouth and make sure he learns good hygiene and hand-washing habits. Those with an infection should also avoid contact sports, kissing and touching the sores.
__________________
You are my forum, my only forum, you make me happy, when skies are grey... Sex health related questions click here. WOMEN'S CHARTER click here Sg law on sex related matters click here Last edited by Big Sexy; 27-01-2016 at 09:25 AM. |
|
#8
|
||||
|
||||
|
Re: All you need to know about Gential Herpes
About shingles
Source: The Star/Asia News Network Monday, 23 | 11 | 2009 By DR Y.L.M http://www.healthxchange.com.sg/news...-shingles.aspx MY father experienced a very painful rash on his back, concentrated on just one patch of his skin. The doctor told him this was shingles. What is shingles? I have heard the term before but I don't quite know what it is. Shingles in a skin rash caused by the virus that also causes chickenpox. It is also called herpes zoster. The virus is called varicella zoster, and it belongs to the herpes group. If it is caused by the same virus that causes chickenpox, then why do some people get chickenpox and others get shingles? Shingles usually occurs years after you get chickenpox. Once you have had chickenpox, you are immune to getting chickenpox again. But the varicella virus may still remain in the body's nervous system - in particular, the nerves. Under certain conditions, such as stress, immune deficiency (like with AIDS, or a cancer patient on chemotherapy drugs), the body's immune system is suppressed. The virus can then be reactivated and cause shingles. And once you have suffered from shingles, you are more likely to get it again. In fact, one out of every three people who has had one episode of shingles are going to get a recurrence. In the US, up to a million people get shingles every year. Shingles commonly occur in people above age 60, however. Since shingles is called herpes zoster, is it some sort of herpes? I don't like the word "herpes". It denotes a sexually transmitted disease. Shingles may be called herpes zoster, but it is not synonymous with the disease, herpes, as you know it. The virus that causes mouth sores and genital lesions is another type of herpes virus. Shingles is contagious. If you have shingles, you can spread it easily to another person who has not had chickenpox. The strange thing is - these people catch chickenpox instead, and not shingles! If I have shingles, when will I know if I am contagious. How long do I have to stay away from my loved ones? You have to stay away from your loved ones for as long as you have new blisters forming and old blisters healing. It's pretty much similar to the duration of quarantine for chickenpox. Only when all your blisters crust and the virus can no longer be spread can you go out and mingle with people who have not yet had chickenpox. What is the difference between chickenpox and shingles? How can I tell one from the other? It's quite easy. The rash of chickenpox appears all over the body, but the rash of shingles appear only in one patch of the skin. Before a rash even appears, you may feel a burning pain on a patch of your skin, and it may become very sensitive. This can go on for several days, up to a week. During this time, you are actually not sure what you are getting. Then small blisters on a red patch begin to appear. New blisters come up. This happens for three to five days. The patch of skin involved is the patch serviced by a particular nerve, the same nerve that hosts the varicella virus that has lain dormant all these years in your body. Shingles is likely to affect the nerves of your body that service the patches/bands of skin on your trunk or back. These bands are called dermatomes. So the blisters will only appear on the dermatome. Usually only one dermatome is involved. Like chickenpox, the blisters itch, pop, ooze out liquid, and then crust over as healing begins. This whole process may last up to four weeks. There is one variant of shingles where pain is present, but the blisters never appear. Is shingles dangerous? That depends on where the shingles is affecting you. Usually there are no complications. But sometimes when you scratch too much and bleed, your blisters can get infected with bacteria, then you can have cellulitis. Or if shingles affect your face, particularly in the region of your forehead and nose (once again, a dermatome serviced by your fifth cranial nerve), your eye can be affected. Is there any medicine for shingles? Do I just have to suffer quietly until it goes away? There are definitely antiviral medication for shingles. Acyclovir and a similar family of drugs should be taken early, especially within three days of the first appearance of the rash.  
__________________
You are my forum, my only forum, you make me happy, when skies are grey... Sex health related questions click here. WOMEN'S CHARTER click here Sg law on sex related matters click here Last edited by Big Sexy; 27-01-2016 at 09:28 AM. |
|
#9
|
||||
|
||||
|
Re: All you need to know about Gential Herpes
Herpes labialis
Cold sore; Fever blister; Herpes simplex - oral; Oral herpes simplex Source: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001631/ Herpes labialis is infection of the lips, mouth, or gums with the herpes simplex virus. It leads to the development of small, painful blisters commonly called cold sores or fever blisters. Causes, incidence, and risk factors Herpes labialis is a common disease caused by infection of the mouth area with herpes simplex virus type 1. Most people in the United States are infected with this virus by age 20. The initial infection may cause no symptoms or mouth ulcers. The virus then remains dormant (asleep) in the nerve tissue of the face. In some people, the virus reactivates and produces recurrent cold sores that are usually in the same area, but are not serious. Herpes virus type 2, which usually causes genital herpes and can infect babies during birth to infected mothers, can also cause herpes labialis. Herpes viruses are contagious. Spread may occur through intimate and personal contact, or through contact with infected razors, towels, dishes, and other shared articles. Occasionally, oral-to-genital contact may spread oral herpes to the genitals (and vice versa). Symptoms The first episode may be mild or severe. It usually occurs in children between 1 and 5 years old. * First symptoms usually appear within 1 or 2 weeks, and as long as 3 weeks, after contact with the virus. Sore throat and fever that can last up to 5 days may occur before the blisters appear. There may also be swollen glands in the neck. * First episode may last 2 to 3 weeks. The lesions may be on the gums, in the mouth and throat, or on the face. It may hurt to swallow. Later episodes are usually milder. * May be triggered by menstruation, sun exposure, fever, stress, or various other unknown causes. * Warning symptoms of itching, burning, increased sensitivity, or tingling sensation may occur about 2 days before lesions appear. An outbreak usually involves: * Skin lesions or rash around the lips, mouth, and gums * Small blisters (vesicles) filled with clear yellowish fluid o Blisters on a raised, red, painful skin area o Blisters that form, break, and ooze o Yellow crusts that slough to reveal pink, healing skin o Several smaller blisters that merge to form a larger blister Signs and tests Diagnosis is made on the basis of the appearance or culture of the lesion. Examination may also show enlargement of lymph nodes in the neck or groin. Viral culture, viral DNA test, or Tzanck test of the skin lesion may reveal the herpes simplex virus. Treatment Untreated, the symptoms will generally go away in 1 to 2 weeks. Antiviral medications taken by mouth may help the symptoms go away sooner and decrease pain. Acyclovir, famciclovir, and valacyclovir are the three oral treatments currently available. Herpes sores often come back again and again. The antiviral medicines work best if you take them when the virus is just starting to come back -- before you see any sores. If the virus returns frequently, your doctor may recommend that you take the medicines all the time. Topical (rubbed onto the skin) antiviral cream (penciclovir andaacyclovir) may be used, but must be applied every 2 hours while you're awake. They are expensive and often only shorten the outbreak by a few hours to a day. Wash blisters gently with soap and water to reduce the spread of the virus to other areas of skin. An antiseptic soap may be recommended. Applying ice or warmth to the area may reduce pain. Tips to prevent future outbreaks include applying a sunblock or lip balm containing zinc oxide to the lips when you're outdoors. A moisturizing balm to prevent the lips from becoming too dry may also help. Expectations (prognosis) Herpes labialis usually goes away by itself in 1 to 2 weeks. It may come back. Infection may be severe and dangerous if it occurs in or near the eye, or if it happens in immunosuppressed people. Complications * Recurrence of herpes labialis * Spread of herpes to other skin areas * Secondary bacterial skin infections * Generalized infection -- may be life-threatening in immunosuppressed people, including those with atopic dermatitis, cancer, or HIV infections * Blindness Herpes infection of the eye is a leading cause of blindness in the United States, causing scarring of the cornea. Calling your health care provider Call for an appointment with your health care provider if you have : * Symptoms of herpes labialis that are severe or that don't go away after 2 weeks * Cold sores near your eyes * Herpes symptoms and have a weakened immune system (immunosupression) due to disease or certain medications Prevention Avoid direct contact with herpes sores. Minimize the risk of indirect spread by thoroughly washing items such as towels in hot (preferably boiling) water before reuse. Do not share items with an infected person, especially when they have herpes lesions. Avoid triggers (especially sun exposure) if you are prone to oral herpes. Avoid performing oral sex when you have active herpes lesions on or near your mouth and avoid receiving oral sex from someone who has oral or genital herpes lesions. Condoms can help reduce, but do not entirely eliminate, the risk of catching herpes from oral or genital sex with an infected person. Both oral and genital herpes viruses can sometimes be transmitted even when the person does not have active lesions. 
__________________
You are my forum, my only forum, you make me happy, when skies are grey... Sex health related questions click here. WOMEN'S CHARTER click here Sg law on sex related matters click here Last edited by Big Sexy; 27-01-2016 at 09:29 AM. |
|
#10
|
||||
|
||||
|
Re: All you need to know about Gential Herpes
Herpes simplex
Source: http://www.nlm.nih.gov/medlineplus/e...cle/001324.htm Herpes simplex is a viral infection that mainly affects the mouth or genital area. Causes, incidence, and risk factors There are two strains of herpes simplex viruses: * Herpes simplex virus type 1 (HSV-1) is usually associated with infections of the lips, mouth, and face. It is the most common herpes simplex virus and many people develop it in childhood. HSV-1 often causes sores (lesions) inside the mouth, such as cold sores (fever blisters), or infection of the eye (especially the conjunctiva and cornea). It can also lead to infection of the lining of the brain (meningoencephalitis). It is transmitted by contact with infected saliva. By adulthood, 30 - 90% of people will have antibodies to HSV-1. The likelihood of childhood infection is higher among those with lower socioeconomic status. * Herpes simplex virus 2 (HSV-2) is usually sexually transmitted. Symptoms include genital ulcers or sores. However, some people with HSV-2 have no symptoms. Up to 30% of adults in the U.S. have antibodies against HSV-2. Cross-infection of type 1 and 2 viruses may occur from oral-genital contact. That is, you can get genital herpes on your mouth, and oral herpes on your genital area. A finger infection, called herpetic whitlow, is another form of HSV infection. It usually affects health care providers who are exposed to saliva during procedures. Sometimes, young children also can get the disease. HSV can infect a fetus and cause abnormalities. A mother who is infected with HSV may transmit the virus to her newborn during vaginal delivery, especially if the mother has an active infection at the time of delivery. However, 60 - 80% of HSV infections acquired by newborns occur in women who do NOT have symptoms of HSV infection or a history of genital HSV infection. It's possible for the virus to be transmitted even when there are no symptoms or visible sores. Two-thirds of people with genital HSV infection have recurrences of their symptoms, and one-third have three or more recurrences (outbreaks) per year. HSV is never eliminated from the body, but stays dormant and can reactivate, causing symptoms. Symptoms * Blisters or ulcers -- most often on the mouth, lips and gums, or genitals * Enlarged lymph nodes in the neck or groin (usually only at the time of the initial infection) * Fever blisters * Fever -- especially during the first episode * Genital lesions -- there may first be a burning or tingling sensation * Mouth sores Signs and tests Many times, doctors can tell whether you have an HSV infection simply by looking at the sores. However, certain tests may be ordered to be sure of the diagnosis. These tests include: * Blood test for antibodies of HSV (serology) * Direct fluorescent antibody (DFA) test of cells taken from a lesion * Viral culture of the lesion Treatment Some cases are mild and may not need treatment. People who have severe or prolonged outbreaks (especially if it is the first episode), people with immune system problems, or those with frequent recurrences will benefit from antiviral medications such as acyclovir (Zovirax), famciclovir (Famvir), and valacyclovir (Valtrex). People who have frequent or severe recurrences of oral or genital herpes may choose to continue taking antiviral medications to reduce the frequency and severity of recurrences. Expectations (prognosis) The oral or genital lesions usually heal on their own in 7 to 10 days. The infection may be more severe and last longer in people who have a condition that weakens the immune system. Once an infection occurs, the virus spreads to nerve cells and stays in the body for the rest of a person's life. It may come back from time to time and cause symptoms, or flares. Recurrences may be triggered by excess sunlight, fever, stress, acute illness, and medications or conditions that weaken the immune system (such as cancer, HIV/AIDS, or the use of corticosteroids). Complications * Eczema herpetiform (widespread herpes across the skin) * Encephalitis * Infection of the eye -- keratoconjunctivitis * Infection of the trachea * Meningitis * Pneumonia * Prolonged, severe infection in immunosuppressed individuals Calling your health care provider Call your health care provider if you develop symptoms that resemble a herpes infection. There are many different conditions that can cause similar lesions (especially in the genital area). If you have a history of herpes infection and develop similar lesions, tell your health care provider if they do not get better after 7 to 10 days, or if you have a condition that weakens your immune system. Prevention Preventing HSV infection is difficult because people can spread the virus even when they don't have any symptoms of an active outbreak. Avoiding direct contact with an open lesion will lower the risk of infection. People with genital herpes should avoid sexual contact when they have active lesions. Safer sex behaviors, including the use of condoms, may also lower the risk of infection. People with active HSV lesions should also avoid contact with newborns, children with eczema, or people with suppressed immune systems, because these groups are at higher risk for more severe disease. To decrease the risk of infecting newborns, a cesarean delivery (C-section) is recommended for pregnant women who have an active HSV infection at the time of delivery. 
__________________
You are my forum, my only forum, you make me happy, when skies are grey... Sex health related questions click here. WOMEN'S CHARTER click here Sg law on sex related matters click here Last edited by Big Sexy; 08-05-2011 at 12:35 PM. |
|
#11
|
||||
|
||||
|
Re: All you need to know about Gential Herpes
KKH doctor on STI
Source: Today Tuesday, 27 | 10 | 2009 Source: http://www.healthxchange.com.sg/news...r-on-stis.aspx Could you have it and not know Not all STDs show obvious symptoms IT WAS his first sexual experience with his then-girlfriend. But Eugene (not his real name) ended up getting more than he had expected. Shortly after, his girlfriend told him she had tested positive for genital warts - something she unknowingly picked up from a former sexual partner. Eugene's subsequent check up revealed that he, too, had contracted the infection. "I noticed tiny bumps around my genitals, but I didn't think anything was amiss because I felt no discomfort," said the 25-year old. Contrary to popular belief, not all sexually-transmitted infections (STI) show obvious or hideous symptoms. Hence, it is possible to contract a STI and not be aware of it, said doctors whom TODAY spoke to. "Some sexually transmitted diseases (STDs) may be symptomless," said Dr Christopher Chong, a consultant obstetrician, gynaecologist and urogynaecologist at Gleneagles Hospital. He will be speaking on the topic next month as part of the Women's Health Series - a lineup of women's health talks and workshops launched by the Obstetrical and Gynaecological Society of Singapore in partnership with the People's Association. According to Dr Chong, more than 10 per cent of men and up to 70 per cent of women with gonorrhoea and Chlamydia - two common types of STI contracted by Singaporeans - may not experience any symptoms or discomfort. Other common STIs in Singapore include syphlis, genital herpes, genital wards and Aids. Chlamydia Trachomatis, which affects both the mouth and genital areas, is one of the most common STI afflicting women, accordingly to Dr Wee Horng Yen, consultant and director of the Women's Wellness Centre at KK Women's and Children's hospital. Because the infection can be a silent one, woman may contract Chlamydia from sexual partners who appear healthy, said Dr Wee. In other cases where symptoms do show up, the problem may simply be due to a lack of awareness. "The patient may be unaware as they do not know the symptoms, and some of these can disappear without treatment. But this does not mean that the person is cured," said Dr Chong. While it is not unusual for STI victims to feel anger, anxiousness and even depression, a few may also be in a state of disbelief. "Some are puzzled as to how they could have gotten it, especially if they have a monogamous relationship, and they claim to have been faithful," said Dr Chong. What they don't realise, warned Dr Wee, is that even one unprotected sexual encounter, as in Eugene's case, may have dire consequences. (STI can cause health complications such as brain and spinal-cord damage, blindness, cervical cancer and infertility.) For instance, a man with a history of genital herpes can pass the infection to his wife, despite the fact that he has been faithful since marriage, Dr Wee said. "The man may shed the virus in his semen without him experiencing any symptoms. His wife gets infected, and can get very distressing genital herpes symptoms such as severe genital pain, ulcers and difficulty passing urine," he added. Condoms, said Dr Wee, can greatly reduce the risk of STI. WARNING SIGNS According to consultant obstetrician, gynaecologist and urogynaecologist, Dr Christopher Chong, common STI symptoms include: * genital discharge (from bladder opening or the vagina) * genital rashes, sores and blisters * growths and ulcers around the genitals * swelling of lymph nodes in the groin area
__________________
You are my forum, my only forum, you make me happy, when skies are grey... Sex health related questions click here. WOMEN'S CHARTER click here Sg law on sex related matters click here Last edited by Big Sexy; 07-05-2011 at 12:11 PM. |
|
#12
|
|||
|
|||
|
Re: All you need to know about Gential Herpes
thanks for all these useful info.
I think i got it the 2nd times......funny feeling at the bro's head near the foreskin.small red bubbles, slight itchy feeling... |
|
#13
|
||||
|
||||
|
Re: All you need to know about Gential Herpes
Quote:
Cheers, Big Sexy 
__________________
Honest FRs are always the most preferred FRs 
|
|
#14
|
||||
|
||||
|
Re: All you need to know about Genital Herpes
wow thanks for the valuable information. Bro Big Sexy
will sure up your point when i can. 
|
|
#15
|
||||
|
||||
|
Re: All you need to know about Genital Herpes
Appreciate the research to make us more aware...
|
| Advert Space Available |
 |
| Bookmarks |
| Thread Tools | |
|
|