 |
|
#106
|
||||
|
||||
|
Re: Sexual Health News
Vasectomy reversal: What to expect
https://www.medicalnewstoday.com/articles/318900.php 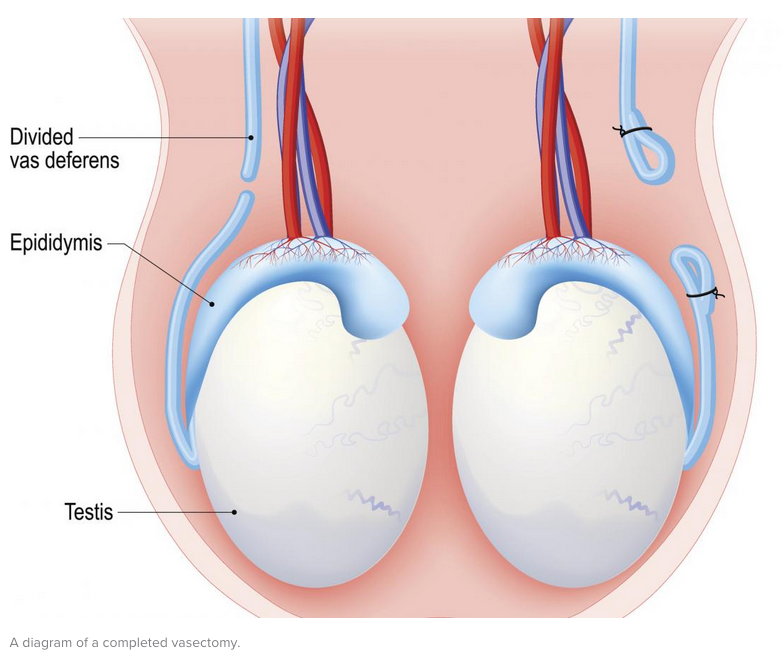 A vasectomy reversal is a surgical procedure that reconnects the male reproductive tract after a vasectomy. A vasectomy is a minor surgical procedure that results in a male no longer being able to make a female pregnant. A vasectomy involves cutting two tubes called the vas deferens, one on either side of the body, so sperm from the testes no longer become part of the semen. While a vasectomy is still considered a reliable and permanent form of contraception, advances in microsurgery have made it possible to reverse this procedure. A vasectomy can be reversed even after a long time, in some cases, 15 or more years, as sperm are continually being produced and remain viable. Overall, around 6 percent of men who have had a vasectomy choose vasectomy reversal later. Contents of this article: Vasectomy and vasectomy reversal procedures What to expect before vasectomy reversal During vasectomy reversal Recovery after vasectomy reversal Risks and complications Outlook Fast facts on vasectomy reversal: A vasectomy reversal reconnects the van deferens that were cut in the vasectomy. Vasectomy reversal is as safe as a vasectomy. A vasectomy reversal does not affect sex drive, and men can typically resume having sex 3-4 weeks after the procedure. Vasectomy and vasectomy reversal procedures Many men may have cause to consider these procedures, to avoid conceiving a child, or because they want their fertility to return due to changes in their personal circumstances. What is a vasectomy? The rate of pregnancy after a vasectomy occurs in less than 2 out of 1,000 women, according to the Centers for Disease Control and Prevention (CDC). Vasectomy is the most effective form of birth control besides complete abstinence from having sex. Vasectomy is an outpatient procedure that takes around 30 minutes. The man is awake the entire time. A small section of the vas deferens is removed from both sides and the ends are sealed. It may take up to 3 months before all sperm are cleared from both vas deferens. During this period, doctors recommend a person uses other forms of birth control, to avoid the chance of an unwanted pregnancy. What is a vasectomy reversal? The reversal of a vasectomy is usually an outpatient procedure involving local or general anesthesia. General anesthesia may be necessary to ensure the patient remains still during the procedure. The success rate for a reversal procedure is around 90 percent, according to a report in the Asian Journal of Andrology. This is based on the success of reopening the vas deferens and the presence of viable sperm. The rate of pregnancy after a vasectomy reversal can be lower than before a vasectomy was done. The success of a vasectomy reversal in achieving pregnancy depends on a variety of factors, including: experience and skill of the surgeon age and fertility of a female partner time since the vasectomy, reversal being harder the longer ago the vasectomy occurred return of moving sperm There are two types of vasectomy reversal techniques: The vasovasostomy reconnects the two sides of the vas deferens. The vasoepididymostomy reconnects the vas deferens to the epididymis, the area above the testes where sperm are stored. It is important to say that a surgeon does not know if a man needs a vasovasostomy or vasoepididymostomy until he is on the operating table. What to expect before vasectomy reversal Doctors perform vasectomy reversals at a surgery center or hospital, but it is still an outpatient procedure with no need for an overnight hospital stay. Before the vasectomy reversal, the doctor will: Take a medical history and do a physical exam - it is important to make sure there are no other health problems that may cause complications during or after surgery. Confirm that healthy sperm can be produced - in most cases, evidence of having fathered a child before is sufficient, but if there is uncertainty, additional testing might be necessary. Review the surgical history - it is important for the surgeon to know about any previous surgeries besides vasectomy or previous injuries that may interfere with the vasectomy reversal. Consider blood tests - these are usually not necessary, but may be recommended for any men with issues of sexual function or an abnormal physical exam. Once a person is in the operating room, he is often put to sleep with anesthesia. During vasectomy reversal During the vasectomy reversal, the surgeon will make a small cut on the underside of the scrotum to expose the vas deferens and free it from the surrounding tissues. The vas deferens is then cut open to examine the fluid inside. Once it is established that there is sperm present, the vas deferens is reconnected to allow the passage of sperm. If the fluid in the vas deferens is thick, it can be an indication of a blockage and that sperm are not flowing. At this point, the surgeon is likely to decide on a vasoepididymostomy as the more appropriate procedure. Many experts believe that the procedure of connecting the vas deferens directly to the epididymis is one of the most challenging in the field of urology and male reproductive microsurgery. The difficulty is due to the small size of the vas deferens - narrower than a piece of angel hair pasta - the even smaller size of the epididymis tube, and the difficulty working on such a small scale. Recovery after vasectomy reversal After a vasectomy reversal, the incisions will be covered with bandages and a person will be advised to wear a jockstrap for support for up to 6 weeks, only removing it when showering. Typically, wetting the surgical area should be avoided for 2 days after surgery. Ice can help with soreness, which may occur for several days after the procedure. If present, stitches should dissolve within 2 weeks. A man should rest for the first 48 hours after the procedure and do as little as possible. Once back home, a man will be advised to limit any activities that cause the testicles to move around too much, such as working out, jogging, or biking for up to 4 weeks after surgery. Sexual intercourse should be avoided until a doctor has given the person the okay. Most men will need to wait at least 3 weeks after surgery. Semen samples are usually collected at 2, 4, and 6 months after surgery to check for presence of sperm. Typically, if no viable sperm are present after 6 months then further surgery may be recommended. Risks and complications While it is safe, there are risks to vasectomy reversal surgery. The most common risk is that full fertility does not resume. Other risks include chronic pain and infection, as well as: inadequate sperm count hematoma bleeding bruising and swelling testicular atrophy, although extremely rare The procedure of vasectomy reversal is safe overall. Complications are fairly unlikely, as long as the surgeon's follow-up instructions are observed and recovery is managed properly. Outlook A person will not know how successful a vasectomy reversal is until their sperm evaluations have been done several months later. Once sperm counts return to adequate levels, the chances of conception improve. |
|
#107
|
||||
|
||||
|
Re: Sexual Health News
Sperm morphology: Tests and results
https://www.medicalnewstoday.com/articles/318963.php Sperm morphology refers to the size and shape of individual sperm. It is one of, but by no means the only, contributing factor to male fertility. Contents of this article: What is sperm morphology? Sperm morphology tests What do test results mean? Other fertility factors Outlook What is sperm morphology? Not all of an individual's sperm look exactly alike. Abnormalities in sperm size and shape can occur in the head, midpiece, or tail. In some cases, these mutations or changes do not impact the sperm's overall functionality. In other situations, the sperm may not be able to move properly or quickly enough to reach, puncture, or enter the egg's membrane. Doctors usually assess sperm morphology during a general semen analysis or fertility test. On its own, an abnormal or low sperm morphology score is typically not an indication of infertility. Sperm morphology tests Sperm morphology tests examine semen samples under a microscope and calculate the percentage of sperm with a normal form (NF) in the total sample. Requirements for a normally formed sperm include: a smooth rimmed, oval shaped head a head that is between 2.5 to 3.5 micrometers (μm) wide and 5 to 6 μm long an acrosome (a membrane with enzymes capable of penetrating the egg's membrane) tip that covers between 40 and 70 percent of the sperm head a head free of large vacuoles (fluid filled organelles) and have no more than two small vacuoles that take up less than 20 percent of the total head midpiece of the sperm (the segment between the head and tail) should be about the same length as the head but much slimmer an uncoiled, 45 μm-long tail that should be thinner than the sperm head and midpiece free from head or tail defects Lab technicians usually process sperm morphology tests by putting a small portion of the semen on a glass slide, letting it air dry, and then staining it with a dye that makes individual sperm easier to see under the microscope. Technicians typically calculate the percentage of NF sperm out of 200 or more sperm in one segment of the sample. Sperm morphology tests can also be assessed using image analysis technology, such as a computer-aided sperm morphometric assessment (CASA). According to the World Health Organization, computer based tests are more precise and reliable than manual tests because of the removed risk of human error. One round of testing is not enough to fully assess semen or sperm quality. There is a high level of variation between different people, as well as between samples from the same individual. Factors such as human error, contamination, mislabeling, and time before processing also make multiple tests necessary. It typically takes three or more tests that produce the same or similar results to confirm qualities such as morphology, vitality, and mobility. What do test results mean? Having a large number of abnormally formed sperm in a sample and a low NF score are signs of a condition called teratozoospermia. The precise range can vary, but typically a normal or healthy sperm morphology range is between 4 and 14 percent NF. A score below 4 percent may mean it takes longer than normal to achieve pregnancy. A result of 0 percent NF usually means in vitro fertilization (IVF) may be necessary for conception. IVF involves the collection of an egg and sperm sample to be combined in a petri dish in the hopes of fertilization. The criteria for sperm morphology was developed less than a decade ago, so there are still a lot of discrepancies in how the test is conducted and results interpreted. It is also important to remember that sperm that is abnormal in size or shape usually still carries healthy genetic material. Many fertile men have a high percentage of abnormal sperm. Most of the studies that have found a link between low sperm morphology scores and reduced fertility rates used IVF subjects and settings. A man whose NF is score below 4 percent should talk to his doctor to rule out the potential for complications and additional health conditions. Doctors specializing in male infertility may help identify a cause for abnormal morphology rates, and in some cases, recommend a course of treatment to improve sperm quality. Other fertility factors Sperm morphology tests are only one component of a general semen analysis. Different laboratories, medical practices, and doctors may include different processes as part of their sperm analysis testing. Other factors and hormones levels typically assessed during semen analysis include: vitality, or the percentage of living sperm motility, or general movement patterns and moving ability of sperm the concentration of the semen the total fluid volume of semen liquefaction, or how quickly semen liquefies to facilitate sperm travel total sperm number or count semen thickness (viscosity) the appearance of the semen semen pH other foreign cells in semen, most often bacteria testosterone sex hormone-binding globulin (SHBG) follicle stimulating hormone (FSH) prolactin estradiol DNA form and function The presence of additional body cells in semen, such as epithelial cells (cells from the male ducts), immune cells such as leukocytes (white blood cells), and macrophages (scavenger immune cells) may also be assessed. Outlook The exact role and influence of sperm morphology on fertility is controversial. The specific requirements for what doctors consider a normal sperm form also vary. Traditionally, if a man had low sperm morphology scores, doctors would likely use assisted reproductive technologies. Doctors also thought that low sperm morphology scores also caused a decrease in overall semen quality and an increase in sperm damage. Increasingly, researchers are finding that morphology may not play as much of a role in infertility as once thought. A 2017 study found that men with 0 percent NF scores were capable of near normal fertility rates. Research has also found that IVF therapies are often ineffective in males with lower than 4 percent NF. Recently developed DNA tests are considered by many researchers and doctors to be a better indicator of infertility and semen quality than a general semen analysis test. Some of the newer DNA tests available to assess the quality of semen include: sperm chromatin structure assay (SCSA) comet assay tunnel assay DNA fragmentation test (Reprosource®) If assisted technologies are used, intracytoplasmic sperm injection, ICSI, where a normal sperm is isolated from a semen sample and injected into an egg, may be a good option for men with low morphology scores. |
|
#108
|
||||
|
||||
|
Re: Sexual Health News
What causes testicle itch? Seven possible causes
https://www.medicalnewstoday.com/articles/319086.php Itchy testicles, also known as itchy balls, can be uncomfortable and very tempting to scratch. In most cases, scratching can make the itch worse. There are a number of potential causes of itchy testicles. Hence, it is important to know what is causing the itch in order to treat the underlying reason for it in the best way. Contents of this article: Seven causes of itchy balls Prevention When to see a doctor Treatment Seven causes of itchy balls Though many causes of itchy balls are benign and easy to treat, there are some more serious conditions that may be responsible. Seven of the most common causes include: 1. Jock itch Jock itch, also known as tinea cruris, is one of the most common causes of itchy balls. Jock itch is a fungal infection that occurs in damp areas of the body, often near or in folds of skin. Jock itch can appear on the feet or genitals. Jock itch often presents as a reddish rash. However, the exact appearance depends on the type of fungus that is causing the infection. Yeast is a common type of fungal infection that causes red, itchy rashes. When a person has a yeast infection on their genitals, they may experience an intensely itchy rash, moist skin, and white-colored discharge near the folds and edge. Other yeast infections may appear dry and flaky. 2. Intertrigo Intertrigo is an inflammatory response to either a bacterial or fungal infection. The resulting rash is often red, raw, and stings. The inflammation most commonly occurs near folds in the skin and moist areas of the body. The scrotum contains many folds and is a moist environment, which makes it an ideal area for bacteria or fungus to grow. 3. Chafing Chafing occurs when constant, prolonged rubbing occurs on an area of skin. This friction can occur during physical activities, such as running or biking. On these occasions, the friction between the legs leaves tiny cracks and inflammation. The resulting rash is often itchy and uncomfortable for the individual. 4. Contact dermatitis Contact dermatitis is an allergic reaction. It is most likely to occur when the skin comes into contact with a new substance, including new body or hair wash, new washing detergent, or a new fabric. Contact dermatitis results in a red, itchy rash that may ooze a white or yellow liquid. The same rash will likely occur in other areas of the body, as well as on the testicles. The thinner skin of the ball sack makes it feel particularly itchy and uncomfortable. 5. Crabs or pubic lice Crabs or pubic lice may also cause itchy balls. Pubic lice cause tiny bites that itch and are uncomfortable. Some people notice lice eggs growing near the roots of their pubic hairs. Others might see the grayish lice, crawling around on their ball sack or around their pubic hair. Crabs may be spread during sexual activity with an infected partner. 6. Genital warts Genital warts is another sexually transmitted infection (STI) that causes an itchy reaction on the balls and other areas of the genitalia. Genital warts are associated with the human papillomavirus (HPV), and although they can be removed, they may reappear in the future, as the virus is not curable. Genital warts can be itchy, but generally, they just resemble small, raised bumps. 7. Herpes Herpes is an STI that causes an itchy rash to appear on the skin. After about a day, the rash turns into one or more blisters that burn. These herpes blisters may eventually burst, leading to painful sores. Prevention Preventing itchy balls requires different precautionary measures depending on the exact cause. For bacterial or fungal infections, a person should keep the balls and genital area clean and dry. A person should consider wearing looser clothing on hot days or during exercise to help the area remain as dry as possible. In cases of allergic reactions, a person should keep a record of known allergens. When something causes the balls or another area of the body to itch, that substance should be avoided. If chafing is the cause, a person can use moisturizers or lubricants to help prevent this rubbing irritation. Moisturizers may also stop itching. Some STIs can be prevented by a person using proper protection during sexual activity. It is also a good idea to know the sexual history of a partner and find out if they have an STI that can be spread during intercourse. When to see a doctor Itchy testicles may not seem very concerning at first. In some cases, a person may know right away what the cause is, and they may not need to seek medical attention. When a rash appears or when itching is persistent and intense, a person should have a doctor rule out certain causes and determine the right treatment. Also, a doctor should examine any rash that changes or starts to ooze. Anyone who suspects they have pubic lice should visit their doctor to appropriate treatment to kill the lice and their eggs. Treatment Similarly to prevention, treatment of itchy balls depends largely on the cause of the irritation. Some common treatments include the following: antifungal creams medicated lotions and shampoos moisturizers and lubricants medication for STIs avoiding allergens Antifungal or antibiotic creams that treat jock itch and other bacterial or fungal infections are a typical over-the-counter treatment. A doctor may also give someone a prescription cream to help treat the infection. Special lotions and shampoo are prescribed to treat pubic lice. These medicated products contain ingredients that kill the lice and their eggs. Moisturizers and lubricants are used to treat itching and rashes caused from chafing. The products help both to prevent and treat a rash. Medication may be prescribed to help reduce outbreaks of an STI. In the case of genital warts, a doctor may burn them off with liquid nitrogen. Avoiding allergens that prompted the rash is the first response to itchy balls caused in this way. The allergic reaction should clear up in about a week. Otherwise, a doctor may prescribe a cream to help recovery. |
|
#109
|
||||
|
||||
|
Re: Sexual Health News
Frequent ejaculation and prostate cancer: What's the link?
https://www.medicalnewstoday.com/articles/319536.php The prostate is a small, walnut-shaped gland that plays an important role in ejaculation. It produces the fluid in semen and helps push this fluid out when a man ejaculates. About 1 in 7 men in the United States will be diagnosed with prostate cancer during their lifetime. As prostate cancer is so common, being aware of the risk factors is important. This article explores whether frequent ejaculation can reduce the risk of prostate cancer. Contents of this article: Is there a link between ejaculation and prostate cancer? Risk factors Reducing the risk Early detection Conclusion Is there a link between ejaculation and prostate cancer? In recent years there have been a number of articles that claim ejaculating more often can reduce the risk of prostate cancer. While these claims might sound like sensationalized headlines, they may be supported in part by scientific evidence. What the research says According to a 2016 study in European Eurology, men who ejaculate more frequently are less likely to develop prostate cancer, compared to those who ejaculate less often. The research from 2016 was a follow-up to a 2004 study, which came to a similar conclusion. Both studies found that the risk of prostate cancer may be reduced for men who ejaculate 21 times or more per month. This was compared with men who only ejaculated 4-7 times a month. Other studies uncovered some conflicting evidence. Researchers disagree whether ejaculating more often makes men of all ages less likely to get prostate cancer. A 2008 study found that frequent masturbation was only linked with a decreased risk of prostate cancer in men over 50. Researchers in this study found that men in their 20s and 30s who ejaculated more often were actually at an increased risk of prostate cancer. In contrast, a 2003 study from Australia found that men who frequently ejaculated as young men had a reduced rate of prostate cancer. More research needed From all the research conclusions that are available, the evidence may point to a link between increased frequency of ejaculation and a man's risk of prostate cancer. However, due to the inconsistent and contradictory conclusions, more research is needed to determine if frequent ejaculation decreases prostate cancer risk in men of all ages. Risk factors Being aware of prostate cancer risk factors can help men understand their likelihood of developing it. According to the American Society of Clinical Oncology, the following factors make it more likely for men to develop prostate cancer: Age: As men get older, their risk of developing prostate cancer increases. Over 80 percent of prostate cancer cases affect men over 65. Ethnicity: Black men are more likely to develop prostate cancer than white men, and they may develop it at an earlier age. Black men also have a higher risk of being affected by aggressive forms of prostate cancer. Hispanic men are less likely to develop prostate cancer than non-Hispanic white men. Family history: Men are at a higher risk of developing prostate cancer if they have close relatives with prostate cancer. Genetics: Certain genetic changes may increase the risk of prostate cancer. Research regarding this potential link is ongoing. Exposure to Agent Orange: Used during the Vietnam War, the U.S. Department of Veterans Affairs has listed this chemical as being linked to prostate cancer. Diet: Researchers believe a man's diet may affect prostate cancer risk, but studies are not conclusive. More research is needed to investigate this possible connection further. Reducing the risk Research from 2014 found the following helped reduce the risk of prostate cancer: stopping smoking exercising regularly taking 5-alpha-reductase inhibitors While the first two lifestyle changes are relatively easy to make, the U.S. Food & Drug Administration (FDA) have not approved 5-alpha-reductase inhibitors for the prevention of prostate cancer. Dietary changes may also help reduce the risk of prostate cancer. Research is ongoing, but the American Society of Clinical Oncology notes the following findings from current studies: diets high in fat may increase the risk of prostate cancer diets high in fruit and vegetables may decrease the risk of prostate cancer However, these dietary changes may need to be made earlier in life to have an effect on a man's risk of developing prostate cancer Early detection Prostate cancer can be detected early using a blood test or with a rectal exam. Diagnosing cancer early can improve the chances of successful treatment. Blood tests may not be the best option for all men, as they can show conditions that do not require treatment. It is a good idea for men over 50 to discuss being tested for prostate cancer with their doctor. Conclusion Research shows the possibility of a link between frequent ejaculation and the risk of prostate cancer. However, further research is needed to understand if ejaculating frequently decreases the risk of prostate cancer for men of all ages. As research is ongoing, it is important for men to read about prostate cancer regularly and discuss their concerns with a doctor. |
|
#110
|
||||
|
||||
|
Re: Sexual Health News
Facts about sperm health and lifespan
https://www.medicalnewstoday.com/articles/319669.php Sperm cells cannot survive for long once they are exposed to the air outside of the body. Precisely how long they can survive depends on the environment that they are released into and how quickly the fluid surrounding the sperm cells dries up. Read on for the answers to some common questions about sperm and sperm survival. Contents of this article: How long do sperm live inside the female body? Can you get pregnant with the withdrawal method? How long do sperm live in a hot tub or bathtub? How long can sperm survive if frozen? How are sperm cells made? What factors can have an impact on sperm health? How to improve sperm health Outlook Sperm lifespan inside the female body After ejaculation, sperm can live inside the female body for around 5 days. The fluid in a woman's reproductive tract has all of the nutrients that sperm need for their survival during that time. Once inside the female reproductive tract, the sperm cells must swim through the cervix and into the uterus to reach the fallopian tubes and female egg. It is a very long journey for sperm cells to make and very few survive. Does the withdrawal method work? The withdrawal method, or when the male "pulls out" of the female before ejaculation, is notoriously unreliable. Before ejaculation occurs, a small amount of semen, also known as "pre-cum," leaves the penis. There is some debate as to whether this fluid contains sperm cells. Until researchers are sure, it is best to assume that pregnancy is possible if this fluid comes into contact with a woman's vagina. According to Planned Parenthood, if the withdrawal method is performed correctly 100 percent of the time, it is about 96 percent effective. However, most people are not able to perform it correctly every time, making the actual effectiveness somewhere around 78 percent. This means that each year, 22 out of 100 women using this method will get pregnant, or around 1 in 5. Withdrawal is more effective when combined with other methods of contraception, such as male or female condoms or spermicide. When using this method, it is also essential to make sure that ejaculation occurs away from the vaginal opening. It is still possible for pregnancy to happen if the sperm spills onto the vagina or vulva. How long do sperm live in a hot tub? In the hot tub, sperm cells do not live for very long at all. The sperm cannot survive for longer than a few seconds after being exposed to the chemicals and hot water. Pregnancy from someone ejaculating into a hot tub would be very rare and likely not even possible. In a warm bath that was not too hot, sperm cells could likely survive for a few minutes. However, it is very unlikely that sperm would be able to find their way through the tub water and into the vagina of a female. Pregnancy occurring in this manner would also be very difficult, if not impossible. However, if a couple were having intercourse in the water, pregnancy would be just as likely because the sperm would enter directly into the female reproductive tract. The outside temperature and physical environment would not have any impact on sperm survival. How long can sperm survive if frozen? Scientists believe that sperm cells can survive indefinitely once they are frozen, as long as the temperature remains stable. At such a low temperature (-196°C), the sperm cells are in a type of suspended animation, which means that all of their essential functions have completely stopped. Men freeze sperm for a variety of reasons. Many do so because they are undergoing infertility treatment, or have cancer or another medical condition that would potentially impact their fertility. Freezing sperm would allow a man to have children even if he lost his fertility due to cancer or cancer treatment. How are sperm cells made? Typically, millions of sperm cells are produced in the testicles every day. During this time, the cells that make up the sperm divide and change. The sperm cells make their way into the epididymis where they finish developing, which can take several weeks. The sperm eventually develops a head and tail, so that it cells start to resemble a tadpole. The head contains all of the DNA or genetic material, and the sperm uses the tail to help it move. What factors impact on sperm health? Many factors that can affect the sperm formation process. Some of the factors that can cause a decreased sperm count or poor sperm function include: Health and lifestyle factors drug or alcohol use job or occupation tobacco use stress overheating the testicles weight Environmental causes exposure to industrial chemicals heavy metals radiation or X-rays Medical reasons infection of the testicles cancer of the testicles swelling of the veins that drain blood from the testicle hormone imbalances physical problems in the tubes that carry sperm through the reproductive system chromosomal or genetic disorders certain medications surgery involving the pelvis, abdomen, or reproductive organs If a couple want to conceive and a man suspects that he has one or more of these risk factors, he may want to consider having a sperm count performed. A doctor may also recommend this procedure if pregnancy does not result after about 6 months. If a man has any of these risk factors, he should try to change them at least 2-3 months before trying to conceive, since that is how long it takes for sperm to fully mature. How to improve sperm health Reducing the above risk factors whenever possible helps to keep sperm cells healthy, especially before conception. There are several things that a man can do to improve the health of his sperm: Maintain a healthy weight: Being overweight or obese can directly impact sperm production and the hormones needed to support the process. Quit smoking: Smoking cigarettes has been associated with a lower sperm count when compared with men who do not smoke. Cut back on alcohol use: Alcohol use can impact testosterone levels, which will, in turn, decrease sperm count Stop using drugs: Anabolic steroids, marijuana, and cocaine have all been linked with decreased sperm production. Take vitamins: Taking vitamins regularly can help to ensure that a man is getting all of the vital nutrients he needs. He should start taking vitamins at least 3 months before trying to conceive. Keep the testicles cool: Spending time in saunas or hot tubs, wearing tight underwear or pants, and placing a laptop computer directly on the lap may all increase the temperature of the scrotum and reduce sperm production. Outlook Sperm live outside the body for different lengths of time, depending on the environment in which they were released. Unless they are deposited into a female reproductive tract, sperm cells are easily damaged and can only survive a few seconds to a few minutes outside of the body. |
|
#111
|
||||
|
||||
|
Re: Sexual Health News
Head and neck cancer: Could oral sex raise your risk?
https://www.medicalnewstoday.com/articles/319819.php New research has discovered that smoking and oral sex are tied to an increased risk of developing HPV-related oropharyngeal cancer, which is a form of head and neck cancer activated by exposure to the human papillomavirus. Although the risk is increased, it is still low; only 0.7 percent of men are ever likely develop oropharyngeal cancer during their lifetimes, according to the new study. The risk of developing the condition was found to be considerably lower among women, non-smokers, and those who had had fewer than five partners with whom they had performed oral sex. Prof. Gypsyamber D'Souza, of the Johns Hopkins Bloomberg School of Public Health, and Dr. Carole Fakhry, of the Johns Hopkins Department of Otolaryngology-Head and Neck Surgery — both of which are located in Baltimore, MD — conducted the research. Their results have been published in the journal Annals of Oncology. Every year in the United States, there are approximately 16,500 cases of oropharyngeal squamous cell carcinoma, which is the most common type of oropharyngeal cancer. More than 11,500 of these are HPV-related. More than 100 different types of HPV exist, but only a few of these are known to cause cancer. HPV16 or 18, for example, triggers most cases of cervical cancer, and HPV16 is known to cause most oropharyngeal cancers. Experts have predicted that by 2020, the incidence of oropharyngeal cancer will overtake that of cervical cancer. "For these reasons," says Prof. D'Souza, "it would be useful to be able to identify healthy people who are most at risk of developing oropharyngeal cancer in order to inform potential screening strategies, if effective screening tests could be developed." She adds, "Most people perform oral sex in their lives, and we found that oral infection with cancer-causing HPV was rare among women regardless of how many oral sex partners they had." "Among men who did not smoke," Prof. D'Souza says, "cancer-causing oral HPV was rare among everyone who had less than five oral sex partners, although the chances of having oral HPV infection did increase with number of oral sexual partners, and with smoking." The study data came from 13,089 individuals, all of whom were aged 20–69 years old, who took part in the National Health and Nutrition Examination Survey. The participants had all been tested for oral HPV infection. To predict the risk of oropharyngeal cancer from oral HPV infection, the researchers used data on oropharyngeal cancer cases and deaths from U.S. registries. |
|
#112
|
||||
|
||||
|
Re: Sexual Health News
Everything you need to know about prostate nodules
https://www.medicalnewstoday.com/articles/319679.php A prostate nodule is a firm, knuckle-like area on the prostate. It may not have any symptoms or may cause bladder infections and chronic pelvic pain. There are several causes of prostate nodules, including prostatitis and prostate cancer. The prostate gland is part of the male reproductive system. It is about the size and shape of a walnut and is found just below the bladder and in front of the rectum. The prostate helps produce semen, which carries the sperm from the testicles through the penis during ejaculation. In this article, we look at the causes, symptoms, and diagnosis of prostate nodules. Contents of this article: What is a prostate nodule? What causes prostate nodules? Prostate changes over time Diagnosis Outlook What is a prostate nodule? A prostate nodule is a firm area that may appear on the prostate. It is raised and hard and feels like the knuckle on a finger. A prostate nodule may be cancerous and, as a result, should be checked by a doctor. A person with a prostate nodule may be referred to a specialist and given a biopsy, which is when a piece of tissue is removed and sent away for further tests. A nodule vs. a tumor A nodule or a tumor on the prostate essentially refers to the same thing - an abnormal growth. However, "nodule" is regarded as a benign growth, whereas "tumor" is used more commonly to refer to cancer. If a person is confused by the terms being used by their doctor, they should ask for clarification, as this can help them get a better understanding of their health. What causes prostate nodules? There are several different reasons a person could develop a prostate nodule. These include: Prostate cancer Prostate cancer occurs when cells in the prostate gland start to grow uncontrollably. Nearly all instances of prostate cancer are a type known as adenocarcinomas. Other, rarer types include: sarcomas small cell carcinomas neuroendocrine tumors transitional cell carcinomas Prostate cancer is the most common form of cancer in men in the United States. It is estimated that in 2017 there will be 161,360 new cases of prostate cancer and 26,730 deaths caused by prostate cancer. Older men are more likely to develop prostate cancer, with 6 out of 10 cases occurring in men aged 65 or over. Not all prostate nodules are cancer, however, and they can be caused by several other conditions. Prostatitis Prostatitis is inflammation of the prostate gland and is often caused by a bacterial infection. Around half of all men are affected by prostatitis at some point in their lives. It does not increase the risk of other prostate diseases. There are four different types of prostatitis: Acute bacterial prostatitis, which is caused by a bacterial infection and comes on suddenly. It is the least common type but the easiest to diagnose and treat with antibiotics. Symptoms include chills, fever, and urine in the blood. Chronic bacterial prostatitis, which is also caused by bacteria. Often, the only symptom is a bladder infection. It is treated with antibiotics but may be recurrent or chronic. Chronic prostatitis, which is also known as chronic pelvic pain syndrome, is the most common type of prostatitis and can come and go without warning. Symptoms include pain and discomfort in the groin and bladder area, which can be treated with anti-inflammatory drugs or alpha-blockers. Asymptomatic inflammatory prostatitis, which does not have any symptoms and often does not require treatment. This type of prostatitis is usually discovered during tests for something else. Prostate calculi This is the presence of stones in the prostate, often called prostatic stones. Doctors believe they are formed either by secretions from the prostate thickening, or when pus and other debris fuse together during an infection. Prostate calculi can be associated with chronic prostatitis and often has similar symptoms. The presence of the stones can lead to inflammation of the prostate, which stops urine exiting the body and can lead to a bacterial infection. Other causes of a prostate nodule include: infarct, an area of dead tissue caused by a loss in blood supply abnormalities in the rectum, such as a hemorrhoid Prostate changes over time The prostate gland tends to grow as men age. An enlarged prostate may squeeze the urethra and make it difficult to urinate. This requires medical attention. The risk of having prostate problems increases with age. The most common prostate problems are inflammation, an enlarged prostate, and prostate cancer. Having one problem does not directly lead to another, however. Symptoms that require medical attention include: passing urine more often than usual having an urgent need to pass urine a reduced flow of urine a burning feeling when passing urine having to get up many times in the night to pass urine Diagnosis A doctor will ask about a person's symptoms and their medical history and may take a urine sample for testing. The standard way to examine the prostate is a digital rectal exam. A doctor will insert a lubricated and gloved finger into the rectum to feel the prostate. The test takes around 10 to 15 seconds. The digital rectal exam will allow the doctor to feel if there is a prostate nodule present. Prostate-specific antigen (PSA) test A PSA test checks for elevated PSA in the blood, which is a protein produced by the prostate. Increased PSA in the blood may be a sign of prostatitis, an enlarged prostate, or prostate cancer. However, some other non-medical factors can also increase PSA. Biopsy If a doctor has any concerns about prostate cancer, they will refer the man to a urologist for a prostate biopsy. Samples from several areas of the prostate will be taken and tested. Treatment will be decided based on the results. Outlook The outlook for a man with a prostate nodule will depend on the cause of the nodule and the health of the individual. If the cause of the nodule is prostatitis or prostate calculi, it will often be treated using antibiotics or other medications. In rare cases, it may be treated with surgery. If the prostate nodule is cancerous, it will be treated using prostate cancer treatments. The outlook for men with prostate cancer varies depending on their age, the stage of the cancer, and their overall health. While it is a serious disease, most men diagnosed with prostate cancer do not die from it. Prostate cancer affects roughly 1 in 7 men during their lifetime. There are currently around 2.9 million men in the U.S. who have prostate cancer. As well as receiving physical treatment, it is essential that people with prostate cancer seek support from those around them, including family, friends, healthcare professionals, and support groups. |
|
#113
|
||||
|
||||
|
Re: Sexual Health News
Curved penis may increase cancer risk
https://www.medicalnewstoday.com/articles/319960.php Peyronie's disease causes the penis to develop a significant curve. Recent research shows that the total cancer risk in these men may be increased. Peyronie's disease is a disorder of the connective tissue in the penis. Also referred to as penile fibrosis, it causes fibrous plaques to grow in the soft tissue. This scar tissue can cause painful erections and erectile dysfunction. It also shortens and curves the penis. It is difficult to know exactly how many people are affected by Peyronie's, but estimates range from 1–23 percent of men aged 40–70. The plaques that develop as part of Peyronie's are not contagious or cancerous, and the exact causes are still not understood. Some cases seem to be linked to an injury to the penis or a series of injuries over time, but this is not always the case. There may also be an autoimmune component to Peyronie's. Peyronie's, genes, and cancer The condition has been shown to run in families and, recently, the genetics involved in Peyronies has received growing attention. Interestingly, some of the genes that have a relationship with Peyronie's disease also appear to be involved in certain types of human cancer. For instance, WNT2, a protein-coding gene, appears to be associated with Peyronie's and also in the progression of some types of cancer. On the back of these recent findings, researchers from Baylor College in Houston, TX, decided to see whether Peyronie's disease is linked to a measurable increase in cancer risk. Dr. Alexander Pastuszak was the lead investigator; their findings were published recently in the journal Fertility and Sterility and presented at the American Society for Reproductive Medicine's annual meeting on 31st October. Data was taken from the Truven Health MarketScan claims database from 2007–2014. This database carries information about health insurance claims made through employers. The incidence of cancer in people with Peyronie's disease was compared against those without the condition and men with erectile dysfunction, who were used as a secondary control. In total, there were 48,423 men with Peyronie's, 1,177,428 with erectile dysfunction, and 484,230 controls, with an average age of 49.8 years. The men were observed for an average of 4 years, accounting for around 7 million total years of follow-up. Increased cancer risk When compared with men with erectile dysfunction, individuals with Peyronie's had a 10 percent increased risk of all cancers. When this was broken down, men with Peyronie's had a 43 percent greater risk of stomach cancer, a 19 percent increased risk of melanoma, and a 39 percent increased risk of cancer of the testis. Quote:
At a press briefing, Dr. Pastuszak explained what they uncovered: "We found that this father and son had a set of genes that predispose them to both genitourinary or urologic cancers, and testis cancer is within that group, as well as stomach cancers." As they delved deeper into their DNA, they saw increases in either the "suppression of tumor suppressor genes or upregulation of oncogenes." Because this is the first time that such a connection has been drawn, more work will need to be done to firm up the findings. The researchers call for more studies looking at potential pathways by which Peyronie's could influence cancer growth and development. Although the exact pattern of interaction between Peyronie's and cancer is not yet known, the authors suggest a new level of caution from doctors treating men with Peyronie's, saying, "additional follow-up of men with PD after diagnosis and treatment of PD may be warranted." Dr. Pastuszak says of Peyronie's and related conditions, "While they're significant in the sexual and reproductive life-cycles of these patients, linking them to other disorders suggest that these men should be monitored for development of these disorders disproportionately in contrast to the rest of the population. Nobody has made these associations before." |
|
#114
|
||||
|
||||
|
Re: Sexual Health News
What are the best ways to increase sperm count?
https://www.medicalnewstoday.com/articles/320010.php Sperm count or total sperm count refers to the average total number of sperm present in one sample of semen. Sperm count is one of the several qualities that are assessed during routine semen analysis and is considered an important factor for fertility. Based on the most current World Health Organization guidelines, a healthy sperm count is 15 million per milliliter (ml) or at least 39 million per sample. A sperm count lower than 10 million per ml is considered abnormal and commonly associated with male infertility. Anything that impacts the hormones that control the production of sperm or acts as an anti-oxidant may aid the healthy development of sperm and help improve sperm count. Overall, factors that influence testosterone levels are thought to have the most significant impact on sperm number and quality. Contents of this article: Ways to increase sperm count naturally Foods to improve sperm count Medications to increase sperm count Fast facts on how to increase sperm count: Exercise and sleep have been shown to improve sperm count. The first recommended line of treatment is to try non-pharmacologic remedies. Smoking has long been known to reduce overall health, sperm production, and quality. Men with very low sperm counts may be prescribed medication. Ways to increase sperm count naturally For several decades, researchers have known that sperm quality and fertility rates have been in decline in most Western nations. According to a 2017 study, between 1973 and 2011 the average sperm count in North America, Europe, Australia, and New Zealand dropped by 59.3 percent. Despite studies identifying the problem, the reasons for this decline and ways to reliably reverse it are still unknown. Several non-pharmacologic remedies have been used by ancient, herbal, and traditional medicines to increase sperm count and overall sperm health for thousands of years. Researchers have shown that most of these remedies influence sperm count in some way. Natural ways to increase sperm count include: 1. Exercise and sleep Several studies have shown that weight loss and exercise in obese and overweight individuals can lead to improved or increased sperm counts. However, the science linking a healthy Body Mass Index (BMI) to a healthy sperm count is still weak. A 2017 study found that performing a 16-week aerobic exercise program of at least 50 minutes of moderate exercise at 50 to 65 percent peak heart rate 3 times weekly, increased sperm volume and concentration in 45 sedentary, obese men. 2. Reduce stress Any form of stress can cause the body to take defensive actions and conserve energy. In times of distress, it makes biological sense for the body to become less concerned with reproduction and more focused on surviving. Reducing stress requires addressing the cause, though factors such as exercise and a healthful diet are thought to lessen the effects of stress. For men who are experiencing severe stress, a doctor may prescribe anti-anxiety or anti-depressant medications. 3. Stop smoking A 2016 study reviewing the results of over 20 different studies with a total of nearly 6,000 participants found smoking consistently reduced sperm count. 4. Avoid excessive alcohol use and drugs The number of studies exploring the link between sperm health and drugs is limited given ethical considerations. However, some researchers have linked the worldwide use of drugs such as alcohol, marijuana, and cocaine to decreased sperm production. 5. Avoid several prescription medications Some prescription medications can potentially decrease the healthy production of sperm. Once a person stops taking the drug, his sperm count should return to normal or increase. Medications that temporarily reduce the production and development of sperm include: some antibiotics anti-androgens anti-inflammatories antipsychotics corticosteroids anabolic steroids (up to 1 year recovery time) exogenous (outside) testosterone methadone 6. Fenugreek supplement Fenugreek has long been used as a natural remedy for poor sperm health, and advocates suggest it may improve sperm count. A 2017 study found that the patent-pending compound Furosap®, which is developed from fenugreek seeds, significantly improved overall semen quality and sperm count. 7. Get enough vitamin D and calcium Researchers are not entirely sure why, but vitamin D and calcium serum appear to impact sperm health. Some studies have shown that low dietary vitamin D intake seems to correspond with lowered sperm count. 8. Ashwagandha Ashwagandha, also known as Indian ginseng, has long been used in traditional medicines as a remedy for several forms of sexual dysfunction. A 2016 study found that 46 men with low sperm counts who took 675 milligrams (mg) of ashwagandha daily for 90 days saw a 167 percent increase in sperm count. 9. Increase intake of antioxidant-rich foods Antioxidants are molecules that help remove and deactivate free radicals and other compounds that damage cells. Several vitamins and minerals have shown to act as antioxidants, and several studies have linked antioxidant consumption with increased sperm count. Antioxidants that may contribute to a healthy sperm count include: selenium vitamin C (ascorbic acid) vitamin E glutathione coenzyme Q10 I-carnitine 10. Increase healthy fat intake Polyunsaturated fats or so-called healthy fats, such as omega-3 and omega-6, are crucial to the healthy development of the sperm membrane. Some studies have shown that individuals should consume these two essential omega compounds in equal quantities for ideal sperm development and antioxidant benefits. 11. Reduce unhealthy fat intake A 2014 study that surveyed 209 healthy Spanish men between the ages of 18 to 23 years of age found that as they increased their consumption of trans fatty acids, their sperm count decreased proportionately. Several studies have also shown that trans fatty acids may impair the ability of long-chain polyunsaturated fats to incorporate into sperm membranes, a critical step in sperm development. 12. Avoid or limit exposure to environmental or occupational toxins and contaminants As the environment and atmosphere become increasingly polluted and congested, environmental factors, such as air quality and toxic chemical exposure, have frequently been linked to reduced sperm health and total count. Avoiding environmental toxins wherever possible also contributes to overall health. It is important to point out that while some studies have shown a link between low sperm count and environmental contaminants, most of them do not support it. 13. Avoid too much soy or foods with non-human estrogen Some foods, especially soy products, contain phytoestrogens (plant estrogen), compounds shown to reduce testosterone bonding and sperm production. Many canned and plastic products are also high in synthetic forms of estrogen. 14. Get enough folate and zinc Consuming folate and zinc in combination has been shown in limited studies to increase overall sperm health, including sperm concentration or total count. Foods to improve sperm count Though supplements are considered a safe way to get the recommended daily intake of most vitamins, minerals, and antioxidants, the body does not always easily absorb them. Most studies suggest that eating foods rich in specific compounds and chemicals allows the body to use them more efficiently. So the best way to increase sperm count naturally may be to increase the consumption of foods high in sperm-friendly nutrients. Foods high in sperm count-boosting nutrients include: walnuts citrus fruits whole wheat and grains most fish, especially wild salmon, cod, and haddock most shellfish, especially oysters vitamin D enhanced milk and milk products dark chocolate garlic bananas broccoli ginseng turmeric asparagus most leafy greens, especially spinach and kale fermented nuts and seeds Medications to increase sperm count A doctor may prescribe medication for men with very low sperm counts or who have additional health factors or considerations. Medications sometimes used to treat low sperm count include: clomiphene citrate oral (Serophene) serophene oral Gonal-f® RFF* Redi-ject® (follitropin alfa or gonal-F) or subcutaneous (under the skin) injections antibiotics if caused by urinary or reproductive tract infection human chorionic gonadotrophin (hCG) (brand names Choragon and Pregnyl) letrozole or anastrozole exogenous androgens |
|
#115
|
||||
|
||||
|
Re: Sexual Health News
Quote:
So Soy is still fine and is a source of plant protein. But like all things, everything in moderation one of the sources https://www.healthline.com/nutrition...rogens-and-men
__________________
downblouse, view from the sky |
|
#116
|
||||
|
||||
|
Re: Sexual Health News
probably...however the problem with such studies are that most are not conclusive... so just read it with pinch of salt..
 Quote:
|
|
#117
|
||||
|
||||
|
Re: Sexual Health News
What are the best birth control pills for PCOS
https://www.medicalnewstoday.com/articles/320055.php Polycystic ovary syndrome is a hormone disorder that causes numerous symptoms, including infertility. Hormonal birth control that contains both estrogen and progestin can help rebalance the hormones, alleviating many of the symptoms. Polycystic ovary syndrome (PCOS) is an endocrine disorder that affects 1 in 10 women of childbearing age. The endocrine system consists of glands that secrete and regulate hormones, such as testosterone and estrogen. Women with PCOS have a hormonal imbalance that causes unusually high levels of male sex hormones. This imbalance changes the way the ovaries function and can cause them to develop many small cysts. Women with PCOS may also not ovulate or do so infrequently. PCOS is a leading cause of infertility. Contents of this article: What are the symptoms? How birth control can affect PCOS Best birth control pills for PCOS Non-pill options for PCOS Takeaway Fast facts on PCOS and birth control: Doctors do not yet have a cure for PCOS. A widely used treatment for PCOS is combination birth control. The symptoms of PCOS vary from woman-to-woman. Birth control pills help regulate a woman's menstrual period, making it more predictable. What are the symptoms? Some of the symptoms of PCOS include: weight gain and obesity insulin resistance causing diabetes symptoms mood changes, problems concentrating, and fatigue acne on the skin excess body hair, notably on the face thinning hair headaches difficulty sleeping irregular periods due to delayed or no ovulation heavy or painful periods Symptoms vary and may be mild or so severe that they disrupt a woman's life. How birth control can affect PCOS With treatment, the symptoms can be managed and may disappear. Hormonal birth control is considered to be combination birth control when it contains two hormones. These hormones are usually estrogen, and a synthetic form of progesterone called progestin. These combination pills can also regulate some hormonal imbalances, by increasing a woman's estrogen levels and decreasing the amount of testosterone her body produces. Due to combination birth control pills containing two hormones that can adjust hormone issues, they are the preferred choice for many prescribing doctors. However, not all women can safely take combination pills. Hormonal birth control pills are safe, but they do present some risks including: A greater risk of diabetes: This is a consideration for women with PCOS who are already at risk for diabetes. A risk of cardiovascular issues: Including dangerous blood clots in the legs. Women with PCOS who are obese may have an elevated risk. If they smoke, the risk rises. Weight gain: Some evidence suggests that birth control pills can cause weight gain, but other studies disagree. Women who are already obese may be reluctant to take birth control pills. Weight gain can make the symptoms of PCOS worse. For some women, a pill known as the minipill may be a better choice. Minipills contain just one hormone, progestin. They are less likely to cause side effects than combination pills. However, when they do cause side effects, these can be the same. Best birth control pills for PCOS Combination birth control pills all work the same way. They prevent the ovaries from releasing an egg and so prevent pregnancy. They also thicken the mucus of the cervix. If the ovaries were to release an egg, this thickened mucus could prevent pregnancy. The same hormones that prevent ovulation can also keep male hormone levels low and raise female hormone levels. Combination pills for PCOS include: Alesse April Aranelle Aviane Enpresse Estrostep Lessina Levlen Levlite Levora Loestrin Mircette Natazia Nordette Lo/Orval Ortho-Novum Ortho Tri-Cyclen Yasmin Yaz Some pills, such as Loestrin, have lower estrogen levels. These low estrogen levels can reduce the severity of some side effects but may also be less effective against symptoms of PCOS. Someone with PCOS should talk to a doctor about the right amount of estrogen based on their symptoms and other risk factors. Pills for painful periods Women who get some relief from combination pills but who continue to experience painful or heavy periods may wish to switch to a pill that causes them to be less frequent. The following pills can make a woman have less frequent periods: Lybrel Seasonique Seasonale Minipills Women who develop unpleasant side effects from taking a combination pill may wish to switch to a minipill. In some cases, doctors recommend that women try a minipill first. Women who smoke, who have a history of cardiovascular problems, who are very overweight, or who are diabetic may have fewer side effects with a progestin-only pill. Combination and progestin-only pills are highly effective at preventing pregnancy. At typical usage rates, which are the imperfect way most women use these pills, they are about 91 percent effective. Non-pill options for PCOS irth control pills are not for everyone, as some women find it inconvenient to take a pill every day. Non-pill combination options that blend progestin with estrogen tend to be the most effective. Progestin-only options may pose fewer risks and side effects. The non-pill alternatives to birth control for PCOS include: Birth control injection: This injects the hormone progestin into a woman's body every three months. At typical usage rates, it is 94 percent effective at preventing pregnancy. Birth control patch: This is applied to the skin and releases both estrogen and progestin into the bloodstream. With typical usage, it is about 91 percent effective at preventing pregnancy. In women over 98 pounds, it may be less effective. Birth control ring: This is worn inside the vagina, where it releases progestin and estrogen. It is 91 percent effective with typical use. Birth control implant: This is a small rod that a doctor inserts under the skin. It releases progestin only and can prevent pregnancy for three years or longer. At typical usage, it is more than 99 percent effective. Intrauterine device (IUD): This device is inserted into the uterus by a doctor and releases the hormone progestin. It is more than 99 percent effective with typical use. Another IUD contains copper only and does not release hormones or help with symptoms of PCOS. Non-hormonal birth control options, such as condoms, natural family planning, or diaphragms, will not help with symptoms of PCOS. Also, women who want to become pregnant must try another type of treatment. Takeaway Hormonal birth control can help with PCOS symptoms, but it is not the only option. Lifestyle changes, such as losing weight and exercising more, may help. Some women also try supplements or special diets. Some other drugs, such as Metformin, may help when birth control does not work. And for women trying to become pregnant, the medication Clomid can encourage the body to ovulate. Women with PCOS should talk to their doctors about their symptoms, and their treatment aims to arrive at a comprehensive treatment strategy. A woman can ask a doctor to refer her to a specialist for further advice. Birth control can be a part of a strategy for dealing with PCOS, but it does not have to be the only option. |
|
#118
|
||||
|
||||
|
Re: Sexual Health News
Can you get pregnant right after stopping the pill?
https://www.medicalnewstoday.com/articles/320097.php Taking the pill does not mean a woman never wants to get pregnant. If the time arrives when she does want to conceive, she may wonder how long it will take her to become pregnant. The answer to this question can depend not only on when she stopped taking the pill but other factors, including age and overall health. Contents of this article: How the pill works What do the studies say? Considerations when stopping the pill Takeaway Fast facts about getting pregnant after stopping the pill: The U.S. Department of Health and Human Services estimate almost 62 percent of women between 15 to 44 years of age use contraception. A variety of birth control pills are available on prescription in the United States. Sometimes taking the pill can conceal menstrual cycle irregularities. Women may not get pregnant right after stopping the pill, as the menstrual cycle reestablishes itself. How the pill works Birth control pills serve several purposes, including: maintaining consistent hormone levels stopping the estrogen peak that causes ovulation thickening cervical mucus, so sperm cannot reach an egg In addition to preventing pregnancy, taking birth control pills offers several benefits to women. These include reduced bleeding and cramping during a menstrual cycle and reduced risk for ovarian cysts. When taken at the same time every day, birth control pills prevent pregnancy for 91 percent of women on combined pills and 95 percent of women on mini-pills, according to the U.S. Department of Health & Human Services. When a woman wishes to conceive, she will stop taking the pill. How long does it take for the menstrual cycle to reestablish itself? According to the United Kingdom's National Health Service (NHS), a woman's period may be irregular for up to 3 months after she stops taking the pill. Doctors call a woman's first period after stopping the pill a "withdrawal bleed" where she may experience bleeding patterns that are different from her period while on the pill. Doctors call the next period a woman has "a natural period" that is more like her typical period. It is possible that an irregular menstrual cycle, or reestablishing a natural menstrual cycle off the pill, can affect a woman's ability to conceive. What do the studies say? Taking oral contraceptives can result in a short-term delay in achieving pregnancy of 2 to 6 months when a woman stops taking the pill, compared to other contraceptive use, according to a 2013 Danish study published in the journal Human Reproduction. The study included 3,727 women, aged 18 to 40 years. The participants were asked to complete a questionnaire on a monthly basis for 12 months to determine if pregnancy occurred. The researchers also found that women who had used birth control pills for longer rather than shorter time periods were more likely to get pregnant. Similarly, long-term use had no negative effect on the probability of getting pregnant. The study also found that women who had used birth control pills, starting younger than age 21 years old, were less likely to get pregnant when compared to women who started taking the pill after the age of 21 years. The researchers theorized that younger women starting birth control pills might have more irregularities in their menstrual cycle compared with women starting birth control pills later. An older research study published in the 2009 issue of Obstetrics & Gynecology, found that previous use of oral contraceptives does not affect conception in the short-term or during a one-year period after trying to conceive. Considerations when stopping the pill Examples of the factors that impact the likelihood of conceiving after ceasing the contraceptive pill include: A woman's overall health: Factors, such as thyroid disorders, pituitary gland disorders, or polycystic ovary syndrome (PCOS), can affect the chances of conceiving. Women who are obese or excessively thin also may have difficulty conceiving. A woman's reproductive health: Women who have a history of pelvic infections, blocked fallopian tubes, or endometriosis may have greater difficulty conceiving. A man's reproductive health: Low sperm counts can affect a couple's chances of getting pregnant. How often a couple has sex: "Regular" sex when trying to conceive is usually having sex every 2 to 3 days. Having sex less frequently is less likely to result in pregnancy. A woman's age: Rates of pregnancy decline after women reach the age of 35 years. According to the NHS, 92 percent of women ages 19 to 26, will conceive within 1 year of having unprotected sex. An estimated 82 percent of women, 35 to 39 years of age, will conceive within 1 year after having unprotected sex. Most obstetricians use the 1-year mark of having unprotected sex as a milestone in fertility assessment. If a couple has not conceived after trying for 1 year, they may wish to see an obstetrician for further evaluation. Takeaway Many factors go into getting pregnant. While stopping the pill is an important step, so is making sure a woman's body is in the best possible health to conceive. Additional steps a woman can take to ensure a healthy pregnancy include: prenatal vitamins or folic acid supplements to avoid birth abnormalities stopping smoking refraining from drinking alcohol keeping stress to a minimum While stopping the pill may temporarily extend the time to conception, some women will get pregnant immediately after they come off the pill. Therefore, it is vital for a woman to be ready to take care of her body during her pregnancy, as soon as she and her partner begin trying to conceive. |
|
#119
|
||||
|
||||
|
Re: Sexual Health News
What is herpes gladiatorum?
https://www.medicalnewstoday.com/articles/320202.php Herpes gladiatorum is an infection caused by herpes simplex virus type 1, a virus similar to that which causes cold sores. It is common among those who engage in high-contact sports, such as wrestling, and is also known as mat herpes. Those infected with herpes will carry the virus with them for life as there is no cure. There will be periods where the virus is inactive and no symptoms are present, and times where it is active and causes various symptoms and flare-ups. When the virus is active, the person carrying it is infectious and can spread herpes gladiatorum to others. The virus can be transmitted by skin-to-skin contact and is easily passed from one person to the next. In this article, we examine the symptoms of herpes gladiatorum and the parts of the body that can be affected. We also take a look at diagnosis, treatment, and prevention of the condition. Contents of this article: Symptoms Causes and risk factors Diagnosis Treatment Prevention Outlook Fast facts on herpes: Herpes gladiatorum is triggered by herpes simplex virus type 1 (HSV-1). Between 30 and 90 percent of adults have been exposed to the herpes virus in the United States. Many of these people never develop symptoms. Symptoms The symptoms of herpes gladiatorum vary from person to person. The skin condition can reach any part of a person's body and is particularly dangerous if it affects the eyes. Symptoms tend to appear within 8 days of a person's exposure to someone with the condition. Symptoms of herpes gladiatorum include: fever swollen glands sore throat sores or blisters on the skin, which can be painful a tingling sensation in the affected area headache Blisters and sores that appear as a symptom of herpes gladiatorum can be treated and usually take 7 to 10 days to clear up. When the virus is inactive, people carrying it will not display any symptoms and may not be contagious. However, having no symptoms is not a guarantee that they will not infect others. How frequently flare-ups occur varies, and can be as often as once a month or as infrequent as once a year. A person is most contagious during a flare-up. Complications Though it is rare, there have been cases where the herpes simplex virus (HSV) causes blisters, which then become infected by bacteria. If this happens, the skin infection will need to be treated with antibiotics. There is also a small chance a bacterial infection will spread to different parts of a person's body, including the brain, eyes, liver, or lungs. If this occurs, it is a medical emergency, and urgent medical attention is necessary. Causes and risk factors Herpes gladiatorum is highly infectious and is spread from person to person through skin-on-skin contact. Common ways that herpes gladiatorum can be passed from one person to another include kissing someone who has a herpes cold sore on their mouth, sexual contact, and sharing items, including drinks containers, utensils, or even mobile phones. More commonly, herpes gladiatorum is spread if someone with the virus plays sports that involve them having skin-on-skin contact with others. High-contact sports, including wrestling, rugby, or basketball can cause herpes gladiatorum to spread. This element is why the condition is also known as mat herpes. People with the virus often find that stress can cause flare-ups, as well as periods of illness where the immune system is weakened. While some people carrying the virus can go through long periods without any flare-ups, it is important to remember that a reappearance of symptoms can occur at any time. Seeking advice from a doctor about what precautions to take to avoid infecting others is always advisable. Diagnosis A doctor can examine sores to determine whether someone is carrying the virus. The doctor will often make a diagnosis without further testing, although they may take a tissue sample from the sores to be sent for analysis. If a person does not have sores but has other symptoms of herpes gladiatorum, it is still advisable to seek medical attention and avoid skin-on-skin contact with others. A blood test can be done to confirm whether the virus is present or not. A blood test may also be done if a doctor is uncertain whether a person has herpes or another, similar skin condition. People with herpes gladiatorum have particular antibodies in their blood that can confirm whether someone has the condition or not. |
|
#120
|
||||
|
||||
|
Re: Sexual Health News
Can hepatitis C be transmitted through oral sex?
https://www.medicalnewstoday.com/articles/320253.php Hepatitis C is a type of liver disease that can spread from person to person. It is caused by the hepatitis C virus, otherwise known as HCV or hep C. There is no current vaccine to protect against hepatitis C, although preventive measures can be taken to reduce a person's risk of contracting the disease. Unprotected vaginal and anal sex can lead to contracting sexually transmitted infections (STIs), but people may wonder if the same applies to oral sex. Hepatitis C is a viral disease and is contagious — is it possible to contract hepatitis C from oral sex? Hepatitis C spreads through coming into contact with another person's blood. If infected blood from one person enters another person's bloodstream, that person may become infected. Overall, the risk of transmitting hepatitis C during any type of sexual activity is low. While highly unlikely, it could happen during oral sex if a person with hepatitis C has cracked and bleeding lips and the partner has an open wound. According to the Centers for Disease Control and Prevention (CDC), hepatitis C is not spread through kissing or saliva. Contents of this article: What is hepatits C? Hepatits C and oral sex How is hepatitis C transmitted? Symptoms When to see a doctor Treatment Outlook What is hepatitis C? Hepatitis C is a virus that affects the liver. According to the World Health Organization (WHO), around 71 million people have chronic hepatitis C infections globally. Just under 400,000 people die from hepatitis C-related liver diseases every year. Hepatitis C damages the liver cells, causing inflammation and scarring known as fibrosis, as well as liver cirrhosis. It can also cause liver cancer and liver failure. Hepatitis C and oral sex Currently, there is no direct evidence to prove that hepatitis C is transmitted through oral sex alone. However, a person should still be cautious anytime blood is present because an infection can still occur. If either sexual partner has a break in their skin, there may be a risk of blood passing from one person to the other. Additional risk factors may include: menstruation bleeding from the mouth or gums a throat infection cold sores or canker sores genital warts or herpes damaged and cracked lips The risk of contracting or passing hepatitis C from one person to another during oral sex is very low. This is particularly true of couples in monogamous relationships who have been tested for contagious diseases. Knowing how hepatitis C transfers from one person to another, as well as understanding safer sex practices, can further reduce a person's risk of infection. Risk factors for contracting hepatitis C include: a person has an acute HCV infection a high viral load individuals who have multiple sexual partners not using barrier protection, such as condoms or dental dams, during sexual activity damaging the skin from previous injuries or rough sexual activity already having an STI or HIV How is hepatitis C transmitted? While transmission of hepatitis C through sexual contact is rare, there are many other ways a person can become infected. The hepatitis C virus lives in the blood and certain bodily fluids. Transmission of the virus occurs when an infected person's blood is transmitted to another person. Exchange of semen may also result in infection, though the chances of this are very rare. Additionally, while the hepatitis virus has been detected in saliva, it is believed that antibodies in saliva block the transmission of the virus to others, so the disease is not transmitted through kissing. Besides sexual contact, the most common ways a person can become infected with hepatitis C virus are: injecting drugs intranasal drug use or snorting drugs unregulated or unsanitary tattooing and body piercing being born to a mother infected with the virus sharing razors, toothbrushes, and grooming clippers certain medical procedures breastfeeding, only if nipples are cracked or bleeding; it is not transmitted in breast milk Symptoms Many people who have been infected with the hepatitis C virus do not realize that they have it. However, depending on whether the infection is acute or chronic, symptoms of the disease can include: lack of appetite fever abdominal pain fatigue tenderness of the liver darker urine grey-colored stool joint or muscular pain jaundice (yellowing of the skin and whites of the eyes) depression The majority of people infected will only experience symptoms as the virus progresses and may not experience symptoms when they first contract it. Many infected people only discover they are carrying the virus when they have a routine blood test or try to donate blood. When to see a doctor Although it is often difficult for a person to know that they have been infected with the hepatitis C virus, if they have reason to believe they have been exposed to it, they should get tested as soon as possible. All individuals born between 1945 and 1965 should be tested for hepatitis C if they have not been already. People of this generation are five times more likely to have hepatitis C than other people. There is no clear reason for this, but researchers know that transmission was at its highest during the 1960s–1980s. Diagnosis is made using a blood test to check for specific antibodies that would be present in an infected person. This test is known as the hepatitis C antibody test or anti-HCV test. If a person tests positive for antibodies, doctors will suggest further testing to see whether the hepatitis C virus is currently active. This test is called an RNA or PCR test. It is possible to have a false positive result. This occurs when a person receives a positive anti-HCV test when they do not have the virus. A positive result can also occur if a person has had the infection in the past, but it has already cleared. An RNA test should always be done to confirm whether a person has active hepatitis C. It is also possible for recently infected persons to receive a false negative result when they do have the virus. This is because there may not be sufficient antibodies present in the blood to react with the test early on. If infected, a doctor may refer a person to a liver specialist. Other blood tests and a liver biopsy may be done to determine the level of damage and whether cirrhosis or cancer of the liver has occurred. A wide range of factors determine the treatment options. People with hepatitis C should also be vaccinated against hepatitis A and B, if not previously exposed. Sexually active people should be screened for STIs on a regular basis, particularly if they change sexual partners or have many sexual partners. It may take up to 4 to 12 weeks for hepatitis C to show up in test results. Treatment About 15 to 20 percent of hepatitis C infections will clear up without treatment. In all other people with the disease, hepatitis C will be chronic. It is not clear why some people can eliminate the virus, and others are cannot. If a person is diagnosed with hepatitis C, doctors can prescribe antiviral medications for treatment. Other self-care practices that a person can do during the acute infection include: adequate rest increase the intake of fluids not drinking alcohol eating a healthful diet If a person is unaware they have acute hepatitis C and it develops into a chronic infection, a doctor may recommend other medical treatments. Outlook Hepatitis C is considered a manageable condition. New antiviral drugs have proven effective at fighting off the virus, and living a healthy lifestyle can help to treat hepatitis C effectively. A person with hepatitis C should always take extra precautions during sexual activity to limit the risk of transmitting the disease to someone else. If a person is diagnosed with hepatitis C, making healthy choices and working closely with a doctor means that they can usually manage the virus. |
| Advert Space Available |
 |
| Bookmarks |
|
|
 t Similar Threads
t Similar Threads
|
||||
| Thread | Thread Starter | Forum | Replies | Last Post |
| Non sexual health question | sicknasty | Sexual Health Issues | 7 | 10-01-2015 05:45 AM |
| Sexual Health Issues | Whybother | Sexual Health Issues | 2 | 24-04-2013 07:02 AM |
| DSC Sexual Health Screening | Huluman | Sexual Health Issues | 3 | 23-11-2008 08:57 PM |
| Sexual Health & Well Being | MrDevil | Sexual Health Issues | 10 | 29-03-2004 09:36 AM |
| sexual health mentor | boyrusty2000 | Sexual Health Issues | 31 | 06-08-2003 11:10 PM |